Referral Notes:
- Growing evidence suggests that maternal anti-SSA/Ro antibodies are necessary to cause cardiac neonatal lupus.
- After treatment with the drug rozanolixizumab under a compassionate use designation, a woman in a high-risk pregnancy gave birth to a healthy infant.
- The proof-of-principle trial has enabled a larger multicenter trial of the drug’s potential to prevent maternal transfer of the anti-SSA/Ro antibodies and thus congenital heart block during 89 high-risk pregnancies in women with a previously affected child.
A pregnant woman in her 30s with well-managed lupus erythematosus had a history of three prior pregnancies complicated by neonatal lupus. Despite daily treatment with hydroxychloroquine, one prior pregnancy in 2022 had ended with a fatal case of complete atrioventricular block at 20 weeks of gestation, while a second in 2023 had required the woman’s infant girl to receive a pacemaker.
Roughly half of all women with lupus, Sjogren’s syndrome, or other autoimmune conditions, including the patient, generate anti-SSA/Ro antibodies. In cardiac neonatal lupus, accumulating evidence by Jill P. Buyon, MD, the Sir Deryck and Lady Va Maughan Professor of Rheumatology and director of NYU Langone Health’s Lupus Center, suggests that placental transfer of these maternal autoantibodies can attack the fetal heart in utero. The autoantibodies, she has long hypothesized, are necessary, albeit not sufficient, to cause congenital heart block.
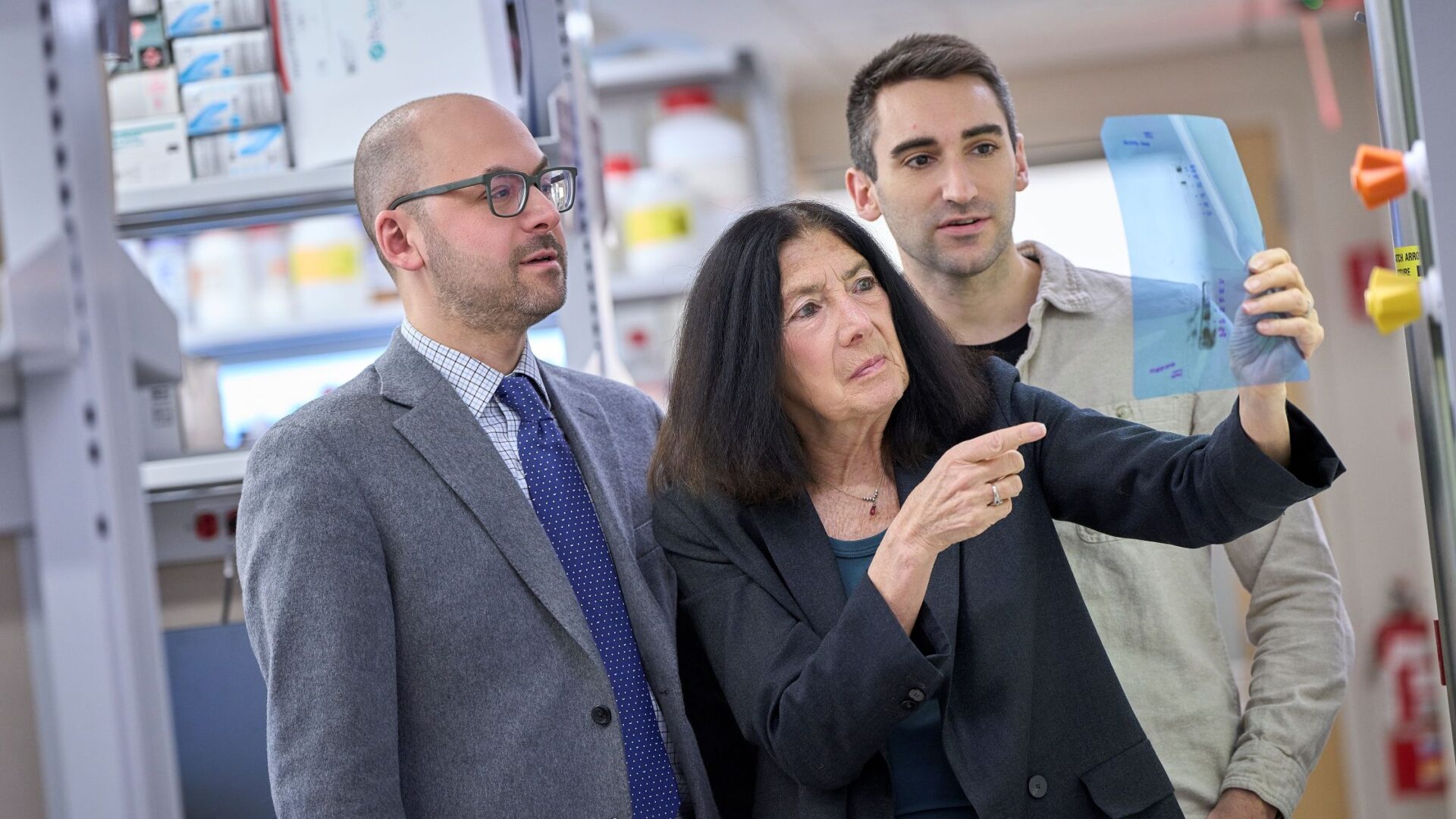
In a new study led by rheumatology fellow Philip Carlucci, MD, researchers including Dr. Buyon and Justin S. Brandt, MD, director of the Division of Maternal–Fetal Medicine, describe a precedent-setting experimental therapy and successful outcome for the woman’s fourth pregnancy in June 2025. Dr. Buyon and colleagues had previously found unequivocal evidence of anti-SSA/Ro antibodies in three fetuses in which congenital heart block had proved fatal before the 25th week of gestation, confirming that the antibodies could be transferred at harmful levels. Those research findings, in turn, suggested a therapeutic strategy.
“This study was born with the idea, ‘No antibody, no disease.’ The concept behind that has been on my mind for 30 years.”
Jill Buyon, MD
“Understanding what the antibody is doing in the fetal heart is obviously very important, but what if you eliminated the antibody?” Dr. Buyon says. Removing the essential contributor might block the disease, regardless of other factors, she points out. “Basically, this study was born with the idea, ‘No antibody, no disease,’” Dr. Buyon says. “The concept behind that has been on my mind for 30 years.”
An Unprecedented Therapy
In the study, published in Annals of the Rheumatic Diseases, the clinical team treated the woman with the drug rozanolixizumab through a compassionate use designation. Rozanolixizumab, a humanized IgG4 monoclonal antibody against the neonatal Fc receptor (FcRn), was approved by the FDA in 2023 for treating myasthenia gravis.
The successful clinical trial for that disease, along with other research, showed that the new medication reduces the overall levels of IgG antibodies and autoantibodies involved in myasthenia gravis. Dr. Buyon and her team hoped that the drug would similarly lower anti-SSA/Ro antibodies as well as block their transport across the placenta.
For the new experimental therapy, the woman received weekly subcutaneous injections of rozanolixizumab from the 14th to the 28th week of her pregnancy, covering the highest-risk period for fetal cardiac injury (from the 17th to the 25th week of gestation). During the treatment period, the mother’s autoantibody levels dropped by roughly 65 percent at week 22 before recovering to near-baseline levels at week 34.
While Dr. Buyon helped to manage the woman’s lupus, Dr. Brandt helped to manage her high-risk pregnancy. “It was really a very synergistic collaboration between us,” Dr. Buyon says. The patient also performed home fetal heart rhythm monitoring three times daily with weekly echocardiograms.
“We did not fully exhale until we heard that the baby was born without heart block or any signs of cardiac neonatal lupus.”
Justin Brandt, MD
Although the patient never experienced serious side effects, the potential risk of infection required a careful determination of when to stop administering the drug. With no signs of congenital heart block, the clinical team ended the weekly injections after her 28th week of pregnancy. “We were cautiously optimistic once the most vulnerable period passed, Dr. Brandt says. “But we did not fully exhale until we heard that the baby was born without heart block or any signs of cardiac neonatal lupus,” he says.
While encouraged by the case’s successful outcome, Dr. Buyon says it’s impossible to know for sure whether the result was due to the blocked transfer of maternal antibodies or some other reason. Nevertheless, she says the forward-thinking nature of NYU Langone allowed the team to complete the unique and challenging study.
“Our dedication to women’s health and to helping families grow was really a driver for us to take a reasonable risk on a drug that had never been used in a pregnant woman before, to try to help a family that desperately wanted to have a heart-healthy child,” she says.
A New Multicenter Clinical Trial
Building on their close partnership, Dr. Buyon and Dr. Brandt teamed up with pediatric cardiologist Bettina Cuneo, MD, at the University of Arizona to propose a larger clinical trial to more rigorously test rozanolixizumab’s potential to prevent recurrent congenital heart block in 89 high-risk pregnancies. The NIH recently awarded the team a $3.7 million, five-year grant to pursue that multicenter trial.
The study, if successful, won’t prove cause and effect either but it could help bolster the hypothesis that the drug can prevent a prerequisite for congenital heart block. Dr. Buyon hopes to get referrals to the trial from other rheumatologists, cardiologists, and maternal–fetal medicine specialists caring for pregnant patients. “This study could be game-changing for these women,” she says.