Referral Notes:
- NYU Langone Orthopedics’ recently assembled system-wide quality council ensures seamless communication and implementation of quality improvement initiatives across sites.
- The MRSA decolonization protocol is applied to nearly all orthopedic surgery patients regardless of MRSA status.
- The regimen includes preoperative CHG wipes and postoperative ethyl alcohol-based nasal antiseptic; high-risk patients with documented MRSA also receive vancomycin.
- The successful implementation relied on hospital in-service training and clear communication of the rationale to patients and providers.
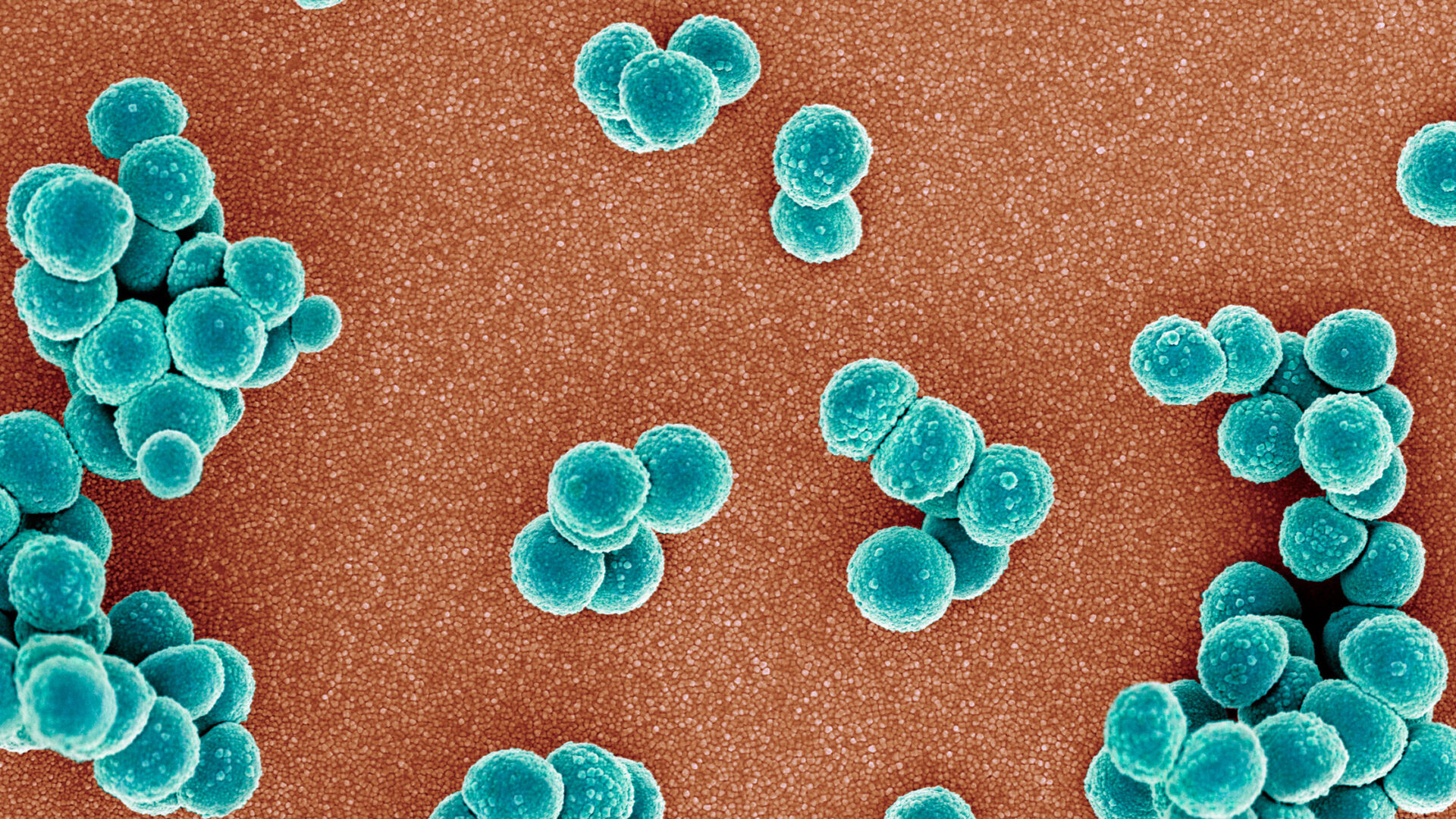
A new quality council and formalized nasal decolonization protocol is helping to minimize the risk of methicillin-resistant Staphylococcus aureus (MRSA) infection in total joint and spine cases.
With the continued expansion of the Department of Orthopedic Surgery, the June 2025 launch of NYU Langone Health’s quality council has provided a system-wide, multidisciplinary channel for ensuring constant communication among the sites and high-quality care for every patient, regardless of location. “As a department, we review evidence-based approaches, protocols, and innovation and then implement changes to improve the way we provide care,” says Joshua C. Rozell, MD, chief of orthopedic surgery at NYU Langone Hospital—Brooklyn.
One of the council’s first acts was to support the system-wide rollout of a standardized screening and nasal decolonization protocol that has long shown its utility in reducing the burden of hospital-acquired MRSA among surgical patients. Lorraine Hutzler, MPA, associate program director of the department’s Center for Quality and Patient Safety, says the goal was to ensure that all locations had the necessary policies, protocols, and medications in place, as well as streamlined testing processes.
Updated Protocol
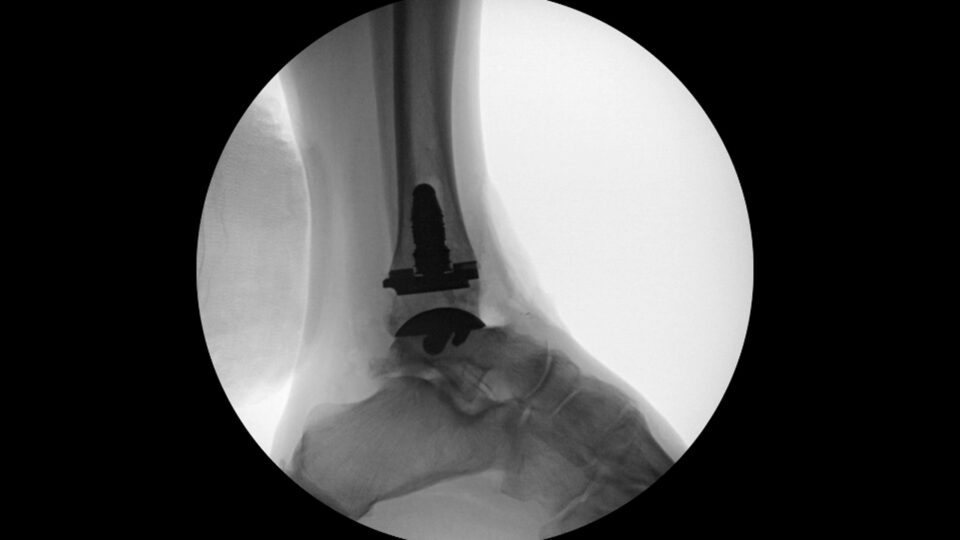
MRSA screening and decolonization is standard of care for patients undergoing joint replacement in an outpatient setting. Richard Savino, MD, chief of orthopedic surgery at NYU Langone Hospital—Suffolk, says the quality council worked to develop a “systemness” approach that made the same protocol consistent across all inpatient settings as well.
“It has eliminated the need to test patients preoperatively, thereby reducing costs without sacrificing quality.”
Joshua C. Rozell, MD
One important step is applying chlorhexidine gluconate (CHG) wipes to patients’ skin in the preoperative holding area. Another is decolonizing their nares in the post-anesthesia care unit, for which the council helped the department test a replacement to povidone-iodine ointment. “Patients often found this procedure uncomfortable and it would result in staining of the nares,” Dr. Rozell says.
An intranasal ethyl alcohol-based antiseptic has offered a quicker, easier, and more comfortable decolonization method. “This protocol is now performed for all patients regardless of MRSA history or testing,” Dr. Rozell says. “It has eliminated the need to test patients preoperatively, thereby reducing costs without sacrificing quality.”
Immediately prior to surgery, patients who have a known diagnosis of MRSA, who have been sent from a nursing home, or who are otherwise at high risk also receive a weight-based dose of vancomycin. “We have found three big factors that increase a patient’s risk of infection: obesity, diabetes, and smoking status,” Hutzler says.
Emphasis on Consistency
As part of the quality council, the department’s Division of Adult Reconstructive Surgery convened representatives from every campus to discuss best practices and standardize protocols for MRSA decolonization. Dr. Rozell worked closely with Dr. Savino and James D. Capozzi, MD, chair of orthopedic surgery at NYU Langone Hospital—Long Island, to implement the protocol at both Long Island campuses. “We then set up in-services for all appropriate staff at all of the hospitals to introduce the new protocol,” Dr. Rozell says.
Beyond the clear goals and easy administration, Dr. Rozell says gaining buy-in from everyone involved in implementing the protocol has been critical to its success so far. “Understanding the ‘why’ is also crucial for providers and patients to make the initiative successful and meaningful,” he says.
“It’s a great comfort for patients to hear, ‘This is how we’re doing it across all systems. It doesn’t matter what site you go to, this is how you’re going to be treated.’”
Richard Savino, MD
Another key to success, Dr. Savino says, has been the supportive attitude that emphasizes collaborative problem-solving. The protocol has been expanded to include most orthopedic surgery patients, offering a “tremendously powerful tool” for conducting research and a highly consistent approach to care, he says. “It’s a great comfort for patients to hear, ‘This is how we’re doing it across all systems. It doesn’t matter what site you go to, this is how you’re going to be treated.’”