Case of the Month
Over the past decade, we have utilized laser, radio frequency, electroporation, high-intensity focused energy, and cryo-therapy at NYU Langone Health to ablate focal disease. Currently, the overwhelming majority of focal therapies (FTs) at NYU Langone are performed using cryo-therapy because of its superior oncological outcomes.
Men undergoing FTs are at risk for developing in-field, out-of-field, or metastatic disease recurrences. In-field disease recurrence develops due to failure to completely eradicate the index focal lesion. Out-of-field disease recurrence develops due to failure to detect co-existing clinically significant prostate cancer (csPCa), or the development of csPCa in the untreated gland. Metastatic disease develops due to pre-existing metastasis or the development of metastasis arising from local recurrences.
In 2017, with James S. Wysock, MD, I initiated an IRB-approved prospective study to rigorously assess functional and oncological outcomes following primary partial gland cryoablation (PPGCA). Our published experience to date has demonstrated the following:
- the ability to reliably ablate the index lesion1
- a low rate of in- and out-of-field disease recurrence at three years2
- no urinary incontinence or rectal injuries3
- an improvement in lower urinary symptoms3
- less adverse impact on sexual function than radical prostatectomy (RP)3,4
We are presenting our five-year oncological outcomes on May 5, 2024, at the American Urological Association (AUA) Annual Meeting. The following case features one of the 298 subjects who met the eligibility criteria for this study. [See the results from the five-year study here.]
Case Presentation
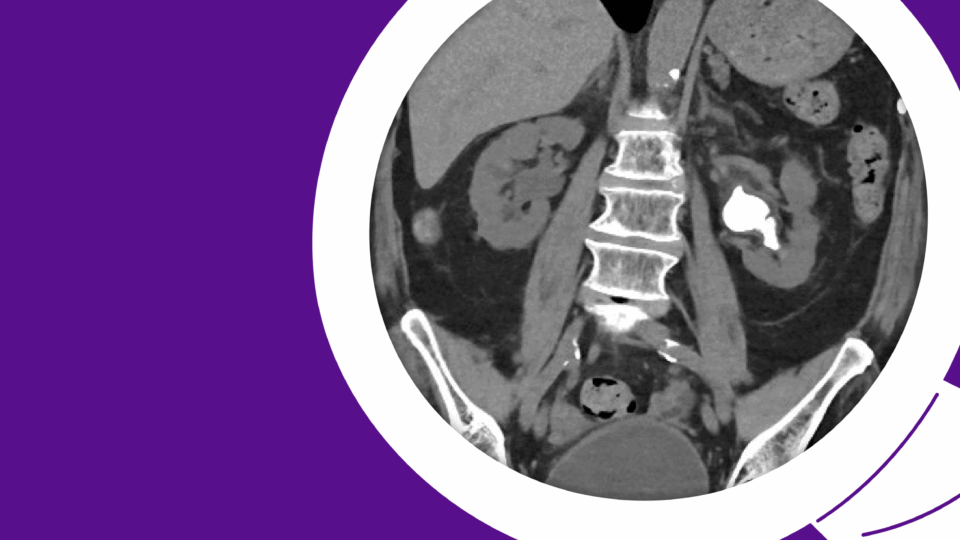
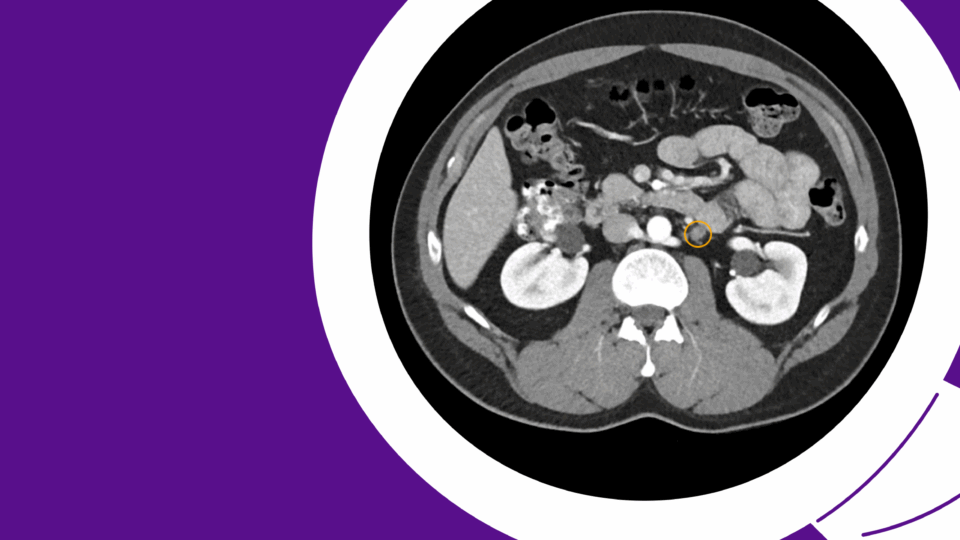
The patient, in his mid-50s at the time of initial presentation in 2018, had a progressively rising PSA level—to 4.4 ng/ml—and a benign digital rectal exam (DRE). He underwent a multiparametric MRI (mpMRI), which showed a 10×5-mm Prostate Imaging–Reporting and Data System (PI-RADS) 4 region of interest in the left medial apical peripheral zone. An MRI targeted, 12 cores systematic biopsy (SB) demonstrated multiple Gleason Grade Group (GGG) 1 and 2 cancers in the targeted and left SB.
We discussed RP, radiation therapy (RT), and FT for managing his focal intermediate risk prostate cancer. Preserving erectile and urinary function and avoiding androgen deprivation therapy (ADT) were the primary factors leading to a shared decision to proceed with PPGCA.
The PPGCA was performed shortly thereafter under general anesthesia using four cryo-probes. The patient was discharged by early afternoon the same day, and the Foley catheter was removed three days post-operatively. The patient returned to unrestricted activities immediately after catheter removal. He never experienced any level of incontinence.
The patient was one of our early PPGCA cases, and the surveillance protocol was the following:
• PSA every six months
• DRE annually
• mpMRI at six months, then at two years, three years six months, and five years; a protocol biopsy, which included sampling the prior MRI target, and any new in- or out-of-field regions of interest suspicious for prostate cancer, and 12 SB.
This table summarizes the functional and oncological outcomes at six months and five years post-treatment.
| Outcome | Six-Month Results | Five-Year Results |
| IPSS | 2 | 0 |
| SHIM | 24 | 23 |
| Semen Volume | Markedly reduced | – |
| Penile Curvature | None | – |
| Climacturia | None | – |
| PSA (ng/mL) | 0.81 | 1.2 |
| mpMRI | Left PIRADS 4 lesion no longer identified, replaced by an ablation cavity. | PIRADS 1 atrophy of the left lobe, no evidence of in- or out-of-field disease. |
| Biopsy Results | Ablation cavity and 6 left SB showed only treatment effect. | Benign |
The patient’s future surveillance protocol will be the following:
• PSA every six months
• DRE annually
• MRI at seven years six months, and 10 years
• protocol biopsy at 10 years
• for-cause biopsy as clinically indicated
Discussion
I have offered and performed FTs since 2012 based on the following observations and assumptions5:
• the aggressiveness of prostate cancer, typically defined by an index tumor
• MRI identifies the index cancer in candidates for PGA
• candidates for FTs rarely have significant prostate cancer outside the ablation zone
• majority of men undergoing RP do not have prostate cancer or metastasis-free survival compared to watchful waiting (WW)
• low-risk and select cases of intermediate-low-risk disease candidates for active surveillance (AS)
• PGA reliably destroys in-field prostate cancer
• preserving quality of life is a high priority for men with clinically localized cancer
There are many energy sources commercially available to ablate prostate cancer. Cryo-therapy is the most versatile energy source and, in our hands, achieves the highest level of oncological control, which is further supported by our five-year outcomes.
A limitation of high-intensity-focused ultrasound (HIFU) is its inability to treat anterior tumors or glands with significant calcifications. We believe the inferior oncological outcomes of HIFU are attributed to failure to achieve confluence of energy in the ablative field, which may be rectified by delivering a second treatment as we do with cryoablation.
The advantage of HIFU over cryoablation is the ability to develop a more precise treatment plan. If double treatment overcomes the inferior in-field recurrence rates, HIFU may become our preferred energy source for small peripheral zone lesions that abut the neurovascular bundle, or those immediately underneath the prostatic urethra.
Our five-year oncological outcomes emphasize the need for active surveillance post-FT. Many of the csPCa recurrent cancers are low-volume Gleason pattern 4, which are amenable to AS based on the PROTECT trial. A salvage ablation is performed for the majority of in- and out-of-field csPCa recurrences requiring intervention. The majority of cases requiring whole-gland salvage treatment are managed with salvage RT.
While the literature indicates salvage RP is safely performed, we believe it is slightly more technically challenging due to the peri-prostatic fibrosis. Unlike salvage RP after radiation therapy, surgical planes are often readily achieved contralateral to the ablation, which facilitates mobilization of the prostate.
In our experience, over two-thirds of men with “focal” intermediate-risk disease will elect FTs over whole-gland treatments. Our patients make an informed decision based on my published functional and oncological outcomes for both RP and FT. The factors influencing the decision to elect FT are:
• availability as an outpatient procedure, with expedited return to work and activities
• avoidance of ADT
• no cases of incontinence or rectal injury
• a less significant impact on sexual function
We now counsel patients with intermediate-risk disease that at five years, they have a 91 percent chance of avoiding the morbidity of whole-gland interventions, while the other nine percent undergo salvage treatments without greater risk than primary intervention.
In 2012, I was confident that FTs would emerge as a reasonable option for intermediate risk disease, especially when preserving quality of life is a high priority. After a decade of critically evaluating both functional and oncological outcomes following FTs, and specifically cryo-therapy, we feel this option should be presented to men with focal intermediate risk disease.
References
1. Wysock et al. (2021). Early oncological control following partial gland cryo-ablation: a prospective experience specifying reflex MRI-guided biopsy of the ablation zone. Prostate Cancer and Prostatic Diseases. DOI.
2. Wysock et al. (2023). Biopsy assessment of oncologic control 3 years following primary partial gland cryoablation: a prospective cohort study of men with intermediate-risk prostate cancer. The Journal of Urology. DOI.
3. Thakker et al. (2022). Early functional outcomes following partial gland cryo-ablation. The Canadian Journal of Urology. PubMed.
4. Wysock et al. (2022). Two-year functional outcomes stratified according to baseline erectile function following partial gland cryo-ablation. Urology. DOI.
5. Kenigsberg et al. (2018). The use of magnetic resonance imaging to predict oncological control among candidates for focal ablation of prostate cancer. Urology. DOI.