Advances in prostate cancer diagnostics and surgical planning have redefined management toward a truly individualized, precision-based approach. Treatment decisions now balance oncologic control with preservation of function and quality of life, rather than adhering to a one-size-fits-all approach.
Preoperative multiparametric MRI (mpMRI) and PSMA PET/CT for unfavorable intermediate-risk, high risk, and very high-risk disease are routinely integrated into operative planning to guide the extent of the dissection, nerve preservation, and urethral reconstruction.1
This case illustrates the application of a precision robotic-assisted radical prostatectomy performed with maximal urethral length preservation and selective nerve-sparing based on preoperative imaging and the patient’s biopsy results. The diagnosis was established through a transperineal MRI/ultrasound (US) fusion-guided biopsy under local anesthesia, which allows for accurate lesion targeting with minimal discomfort while minimizing infection risk and procedural morbidities.2,3
Case Highlights:
- A patient in their late 50s presented with a family history of prostate cancer and an elevated PSA.
- Transperineal MRI/US fusion-guided biopsy under local anesthesia revealed Grade Group 3 disease; pain was minimal at 1 out of 10 by VAS.
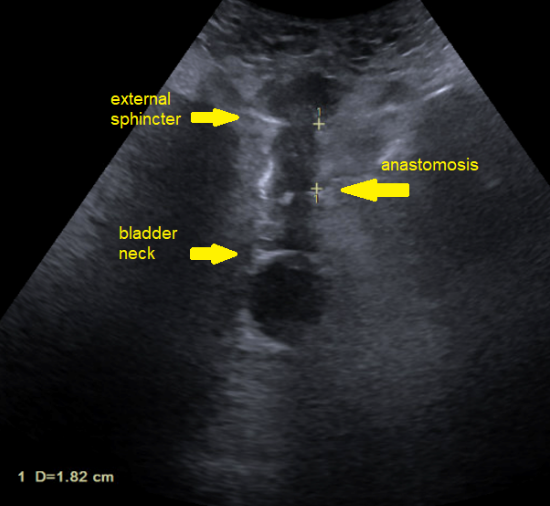
- Robotic-assisted radical prostatectomy featured maximal urethral length preservation and right-sided intra-fascial nerve sparing, with 1.82 cm preserved to the anastomosis and 3.6 cm to the bladder neck; he was discharged same-day.
- Final pathology upgraded the tumor to Grade Group 5.
- He regained continence at catheter removal on postoperative day five, and at three-month follow-up he reported strong erectile function with undetectable PSA (<0.01 ng/mL).
Patient Case
A patient in their late 50s with a family history of prostate cancer presented with a rising PSA, increasing from 4.3 ng/mL in September 2023 to 8.5 ng/mL in December 2024.
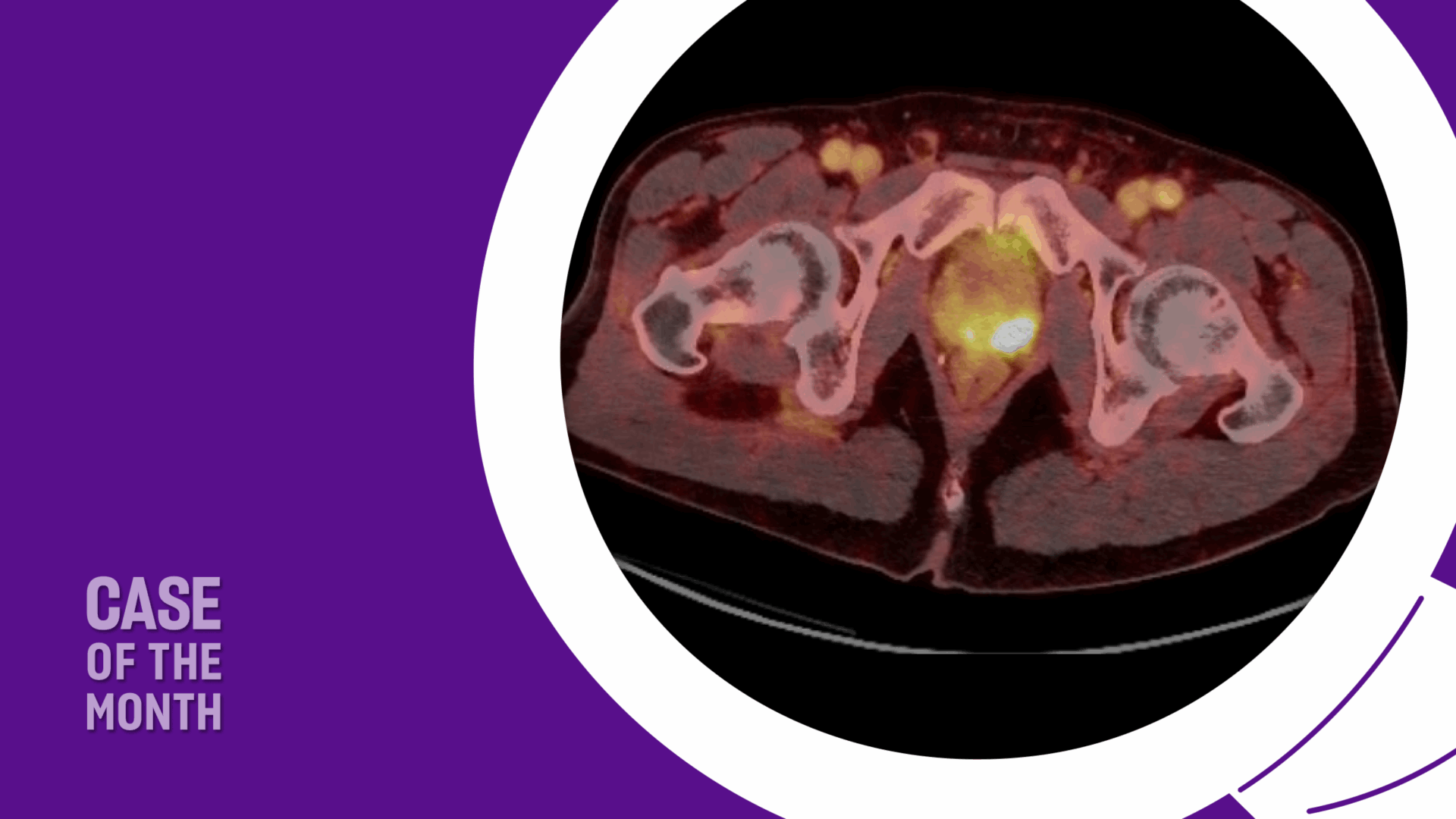
A prostate MRI revealed a 23-cc gland prostate (PSA density = 0.36), a PIRADS 5 abnormality in the left posterolateral base peripheral zone (Figure 1).
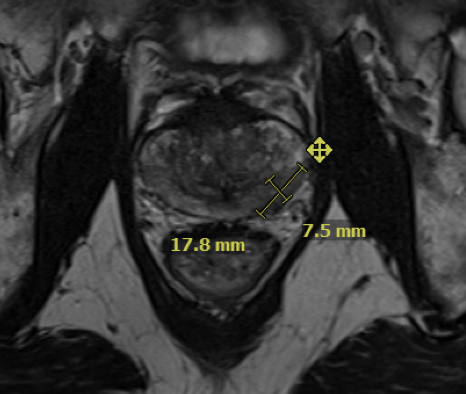
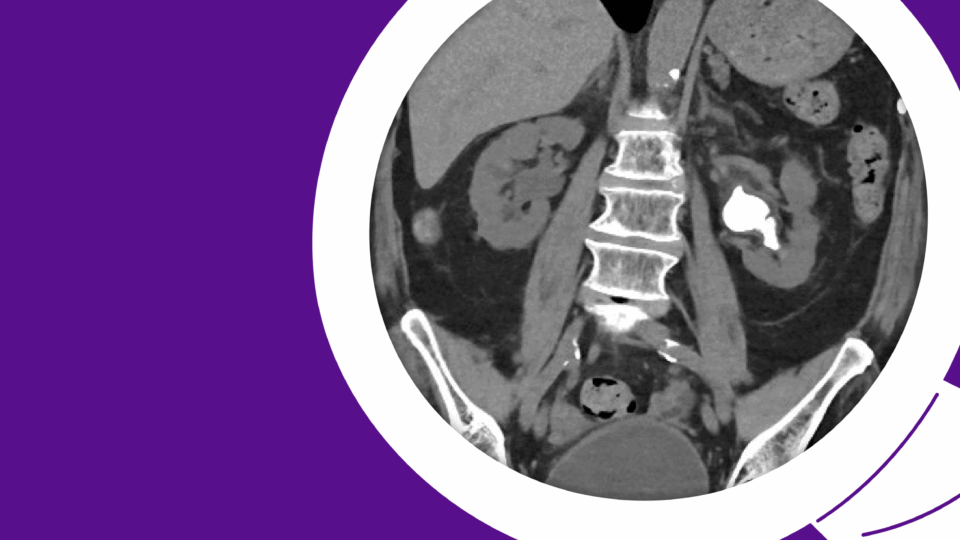
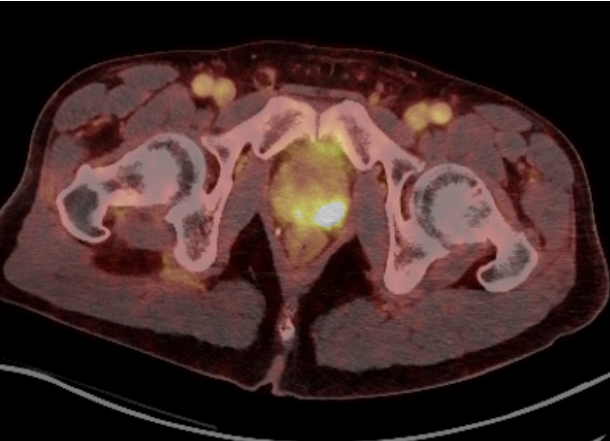
He underwent a transperineal MRI/US fusion-guided biopsy under local anesthesia, reporting a pain score of 1 out of 10 on the visual analogue scale (VAS). His prostate biopsied revealed Gleason 4+3 disease in all four targeted cores of the MRI region of interest. He underwent a PSMA PET/CT which revealed no evidence of metastatic disease, but was concerning for direct invasion of the left seminal vesicle (Figure 2).
He had no past medical histories except for seasonal allergies. His baseline urinary function was normal and he had mild erectile dysfunction which he rated as 9 out of 10 in terms of firmness, and was taking Cialis recreationally.
The patient was adamant about wanting to pursue high intensity focused ultrasound (HIFU), but possible seminal vesicle involvement identified on PSMA PET/CT made him a poor candidate. He ultimately elected to undergo a precision robotic-assisted radical prostatectomy and declined pelvic lymph node dissection given his concern of having lower extremity swelling.
Management
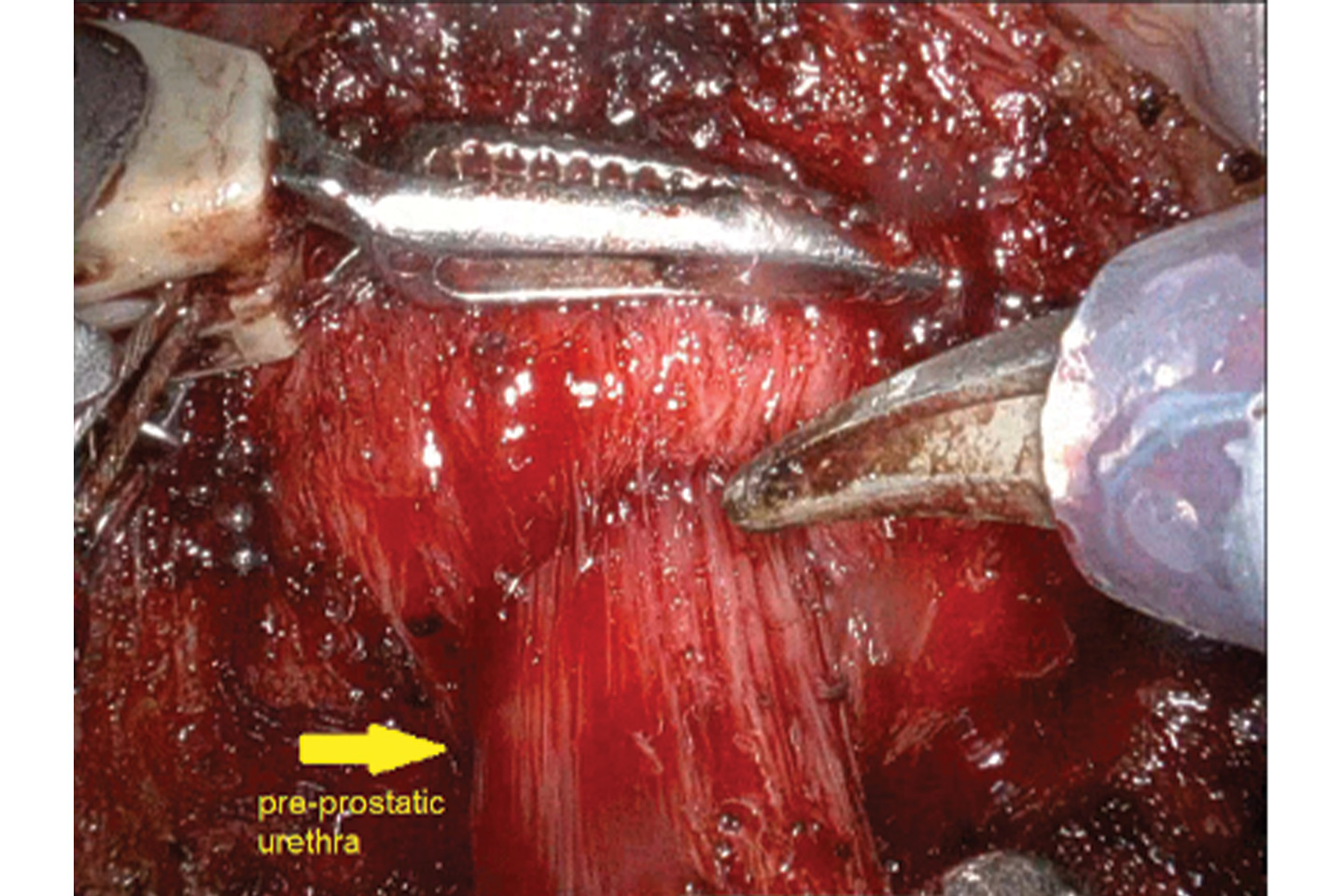
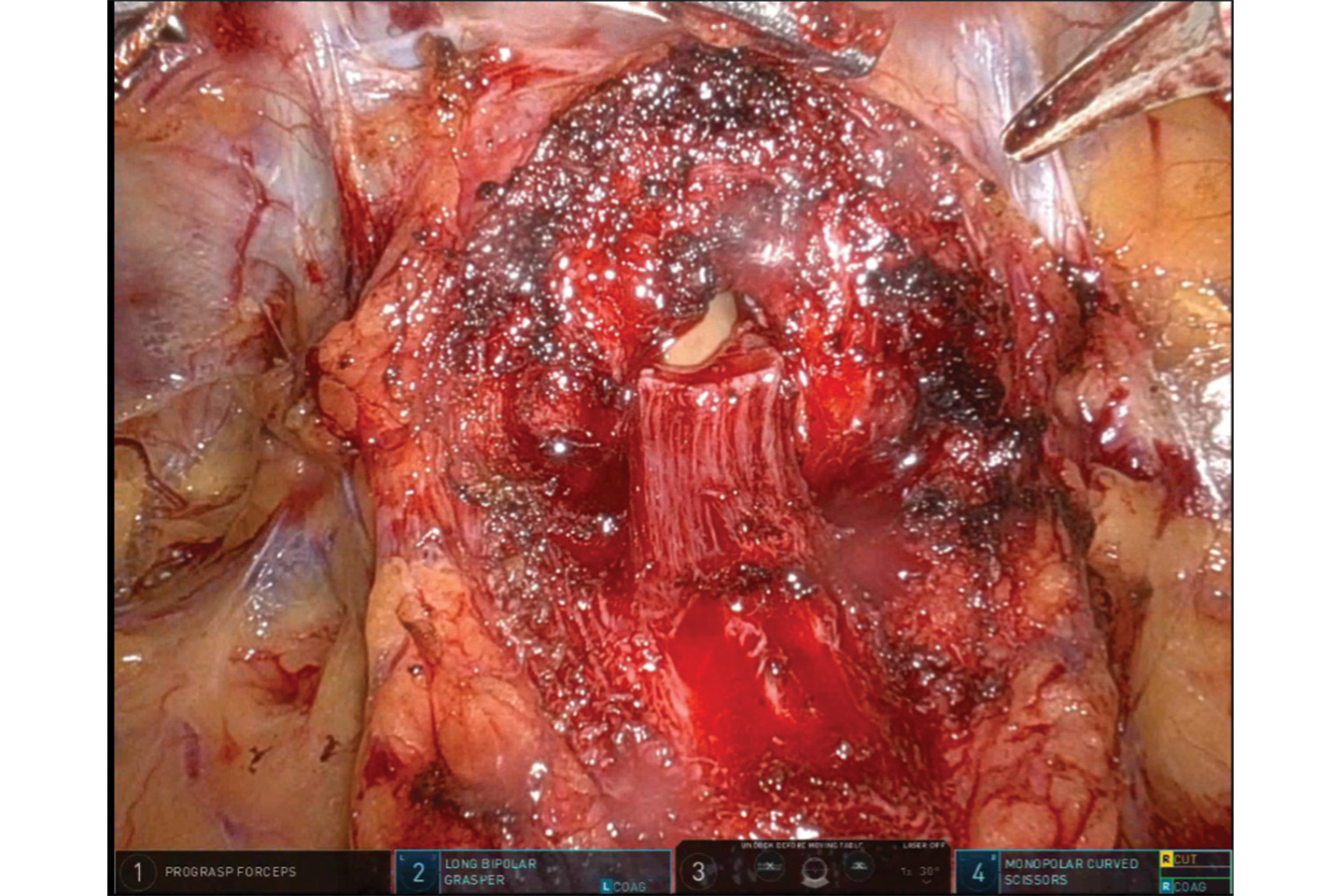
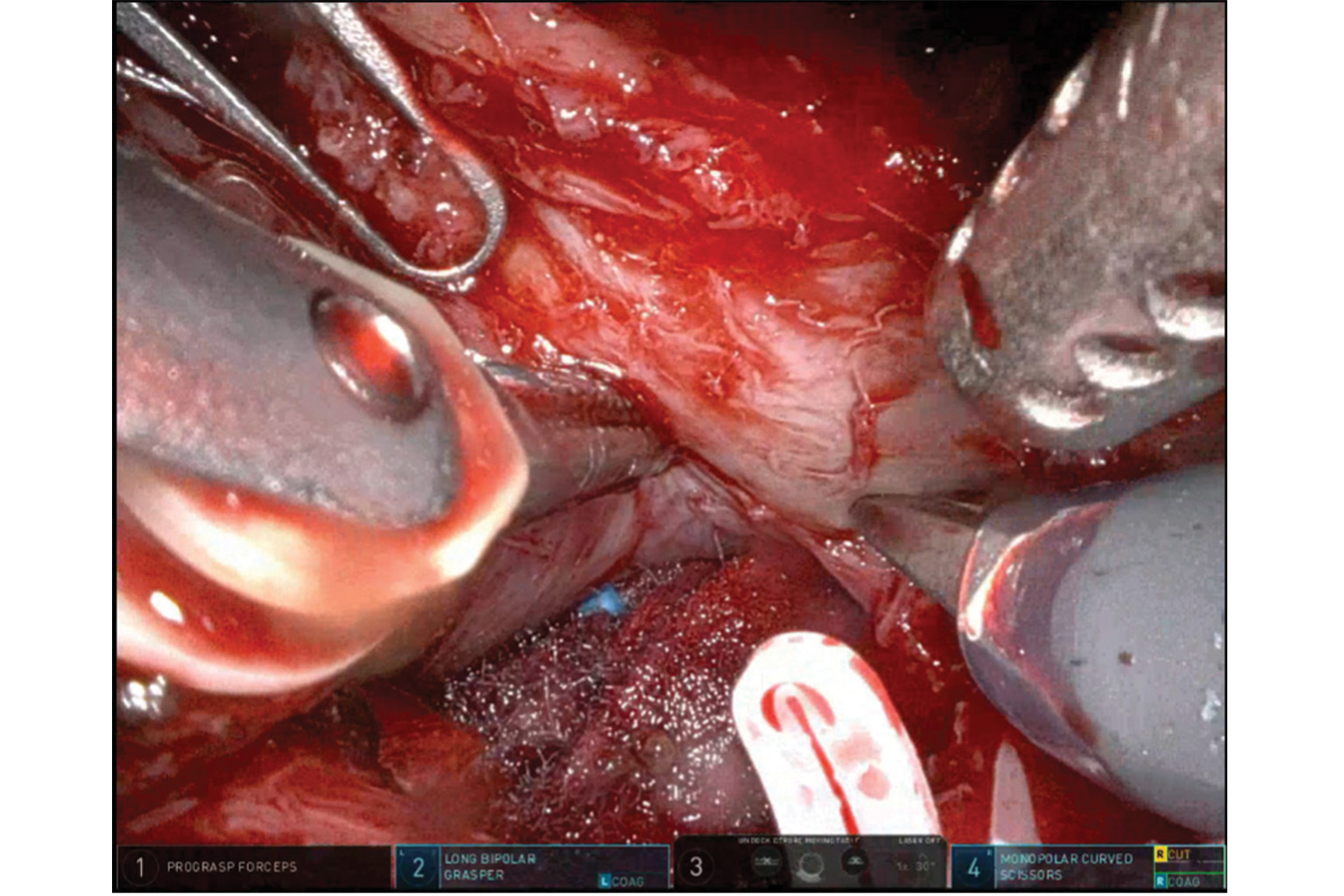
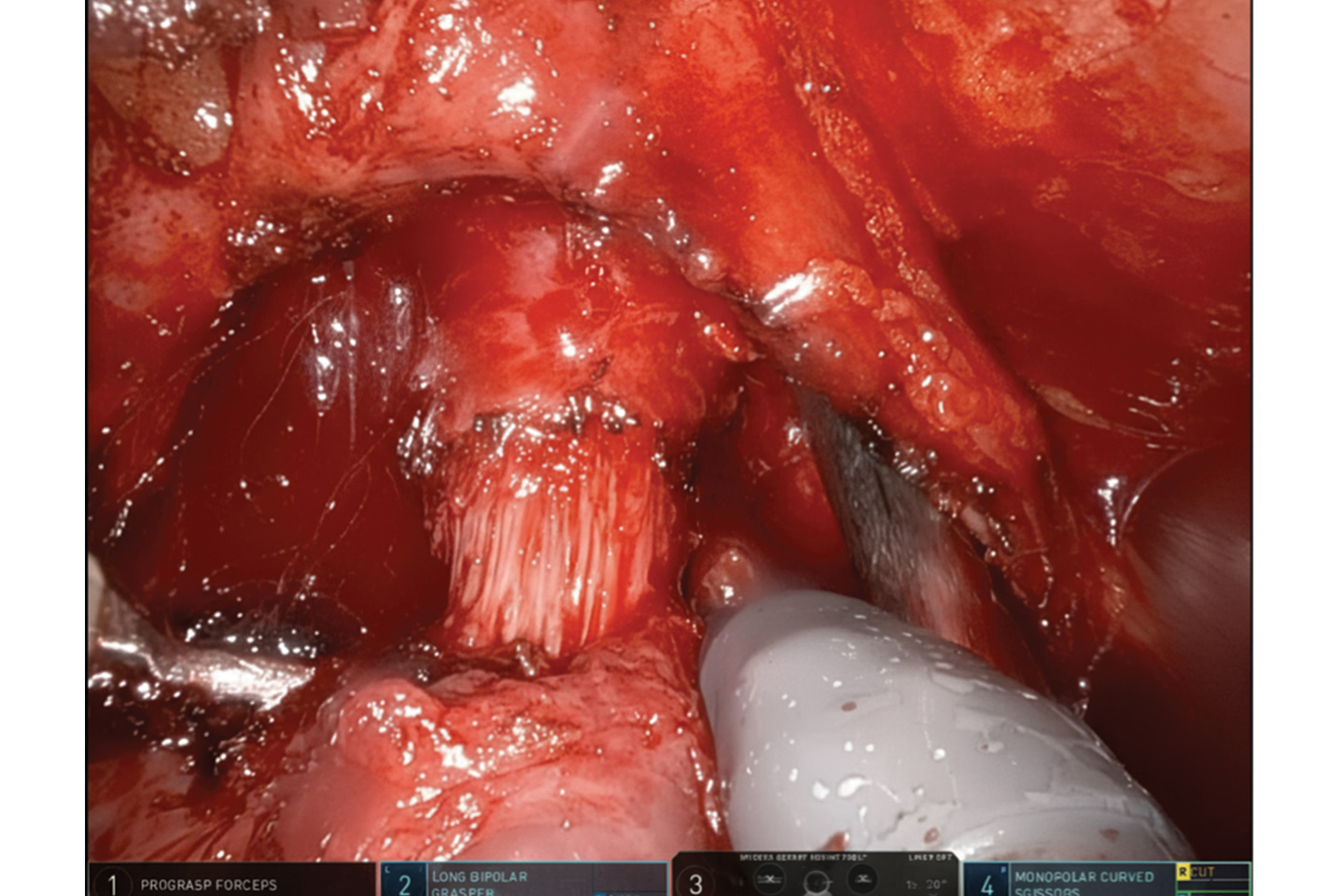
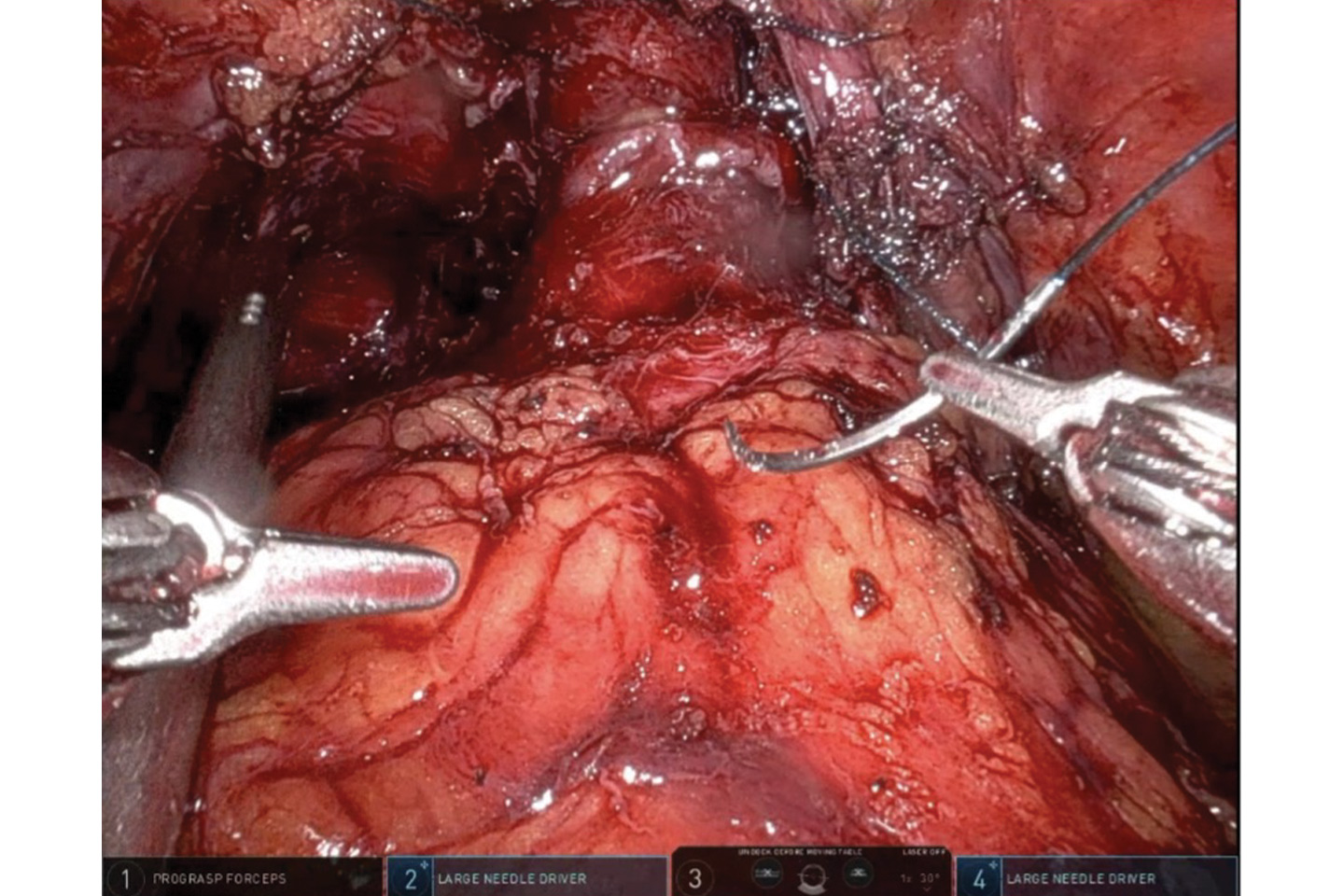
The patient underwent a posterior approach, transperitoneal right-sided nerve-sparing procedure with a urethral sparing and preservation of the anterior and lateral overlying fascia approach (Figures 3–6).
The case was uncomplicated with estimated blood loss of 150 ml. He received IV ketorolac and Tylenol and a direct transverse abdominal plexus (TAP) block. He was discharged from the PACU around four hours after surgery.
His pathology revealed Grade Group 5 (Gleason 5+4), pT3b, Nx, Mx prostate cancer with involvement of the left neurovascular bundle and seminal vesicle, with negative surgical margins. Transperineal ultrasound was performed prior to Foley catheter removal at day five (Figure 7).
He regained complete continence immediately following Foley catheter removal. At the three-month postoperative visit, he was pad free. He reported slightly weaker erections, and continues to take oral phosphodiesterase (PDE) 5 inhibitors to facilitate sexual activity. His PSA was undetectable (<0.01 ng/mL) at three months.
Discussion
Modern prostate cancer management begins with the principle that no two patients are the same. Each diagnostic and therapeutic decision is tailored to the patient’s disease biology, anatomy, and personal priorities, balancing oncologic control with preservation of function and quality of life.
Imaging and Diagnosis. mpMRI has become an integral part of prostate cancer evaluation, enabling a higher detection rate of clinically significant cancer compared with systematic biopsy alone.4 Besides identifying the presence of tumor, mpMRI provides precise intraprostatic localization of the tumor, facilitating targeted sampling and individualized treatment planning.5 When combined with PSMA PET/CT, staging accuracy is further improved, allowing for better surgical planning, and more accurate identification of candidates suitable for focal therapy.1
Biopsy Technique. Transperineal MRI/US fusion-guided biopsy performed under local anesthesia allows for MRI-targeted sampling without antibiotics, greater detection of clinically significant prostate cancer, reduced infection risk, and minimized morbidity. 2,3 Since implementing the awake transperineal biopsy pathway at NYU Langone, we have further enhanced the patient experience through the use of ethyl chloride spray, tactile perineal distraction, and sodium bicarbonate-buffered local anesthesia. These refinements have resulted in a median discomfort score of 1.8 out of 10 on a VAS, based on feedback from 500 consecutive patients surveyed last year.
Surgical Treatment Selection and Personalization. Treatment decision is made by the tumor grade, volume of disease, and focality as determined by imaging and biopsy findings. Management options include active surveillance, focal therapy, and radical prostatectomy. When focal therapy is unsuitable, such as in this case which was concerning for seminal vesical invasion, definitive surgical treatment can be designed using principles of focal therapy that balance cancer control with functional preservation.
Precision Robotic Prostatectomy. Preoperative imaging findings and histopathologic data from the prostate biopsy helps determine the dissection planes and nerve-sparing and urethral preservation strategy. In this case, the left neurovascular bundle was excised due to imaging concerns for extracapsular extension. A Retzius-sparing approach was not performed to allow for a wider excision of the left neurovascular bundle. A maximal urethral preservation technique was employed, sparing an additional 2 cm of the pre-prostatic urethra and the apical prostatic urethra, allowing reconstruction of a tension-free anastomosis resembling a urethroplasty.
This approach facilitates earlier return of continence as seen in this case, although long-term continence outcomes are similar.6 This technique is reversed for cases when preoperative imaging and biopsy confirm absence of cancer near the prostatic urethra to minimize the risk of a positive surgical margin.
References
- Emmett L, et al. Eur Urol. 2021;80(6):682-689. DOI.
- Bryant RJ, et al. Lancet Oncol. 2025;26(5):583-595. DOI.
- Hu JC, et al. Eur Urol. 2024;86(1):61-68. DOI.
- Kasivisvanathan V, et al. N Engl J Med. 2018;378(19):1767-1777. DOI.
- Ahmed HU, et al. Lancet. 2017;389(10071):815-822. DOI.
- Al-Hammouri T, et al. BJU Int. 2025;135(1):171-175. DOI.