Referral Notes:
- Dry eye symptoms in the absence of apparent corneal damage may signal underlying neuropathic corneal pain.
- In severe nerve pain, interventions such as autologous serum drops and nerve-calming medications may provide relief.
- In other cases, ocular misalignments may drive nerve discomfort and respond well to corrective measures like contoured prism glasses.
In October 2025, a patient in her mid-30s presented to NYU Langone Health with eye pain so severe that she described an intense burning sensation and constantly wore a baseball cap to protect herself from glare. Even the slightest bit of wind burned her eyes. Yet when ophthalmologist and dry eye disease expert Mina Massaro-Giordano, MD, examined the patient, her surface corneal epithelium revealed no telltale signs of damage.
For Dr. Massaro-Giordano, the clues pointed toward the more complex, often misunderstood, and regularly misdiagnosed condition of neuropathic corneal pain. While dry eye disease can be accompanied by a wide variety of symptoms such as dryness, irritation, and a gritty or itchy sensation, nerve pain often prompts far more intense descriptions.
“These are patients who say their eyes burn like they’re on fire, or describe a deep, dull ache, or express an extreme sensitivity to light.”
Mina Massaro-Giordano, MD
“These are patients who say their eyes burn like they’re on fire, or describe a deep, dull ache, or express an extreme sensitivity to light,” she says. “When I hear that, I think, ‘This is more than regular dry eye, there’s something else going on.’”
Centralized Pain
In a subset of patients, years of mild or moderate dry eye disease may eventually affect their corneal nerves while leaving little evidence at the surface. “Some patients will have an insult on the surface of the eye, and when you treat that insult or the inflammation it heals,” Dr. Massaro-Giordano says. “For others, it just doesn’t heal completely. In those scenarios, we think that the pain is no longer peripheral, at the ends of the axons, but has become centralized.”
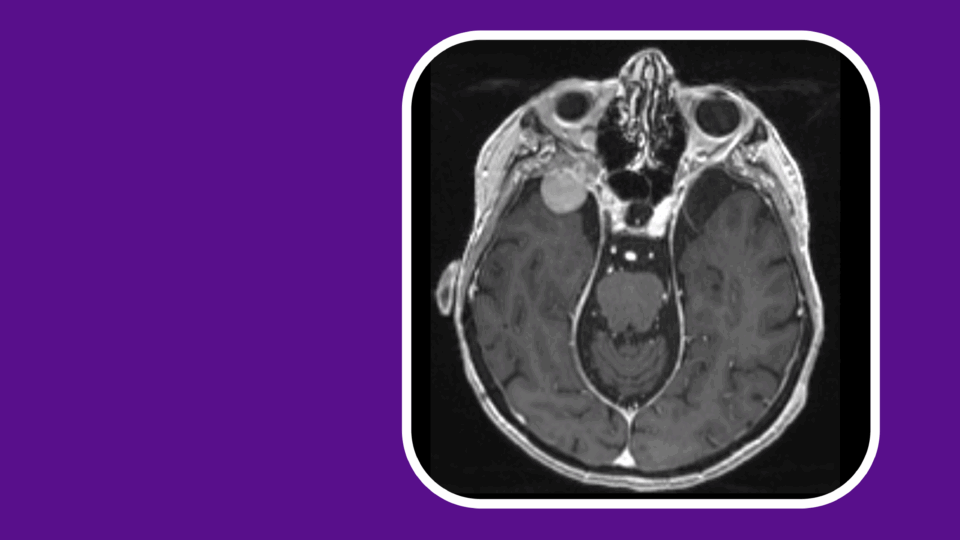
The condition, called centralized pain syndrome, becomes more focalized in the brain. “No matter what the corneal surface looks like, you’ll have abnormal brain signals of pain,” Dr. Massaro-Giordano says.
“The take-home message,” she adds, “is to take eye surface disease seriously early on. If a patient is not getting better and doesn’t have many indicative signs on the surface of their eyes, ophthalmologists should find a way to look at their nerves and treat any underlying inflammation before the condition becomes much harder to treat.”
“The take-home message is to take eye surface disease seriously early on.”
To help relieve the patient’s pain, Dr. Massaro-Giordano first addressed her symptoms at NYU Langone’s Dry Eye Service, using a combination of anti-inflammatory eye drops and autologous serum drops—made from the patient’s own blood—to calm and regenerate damaged nerves.
She then referred the patient to a close collaborator, NYU Langone psychiatrist and pain specialist Franzes Liongson, MD. The patient found relief through a combination of gabapentin and duloxetine, which Dr. Massaro-Giordano says can diminish faulty nerve firing and change the perception of pain.
Correcting a Misalignment
A second patient, in her 60s, presented to NYU Langone in November 2025 with milder symptoms that more closely resembled those of dry eye disease, including a dry sensation, itching, strain, and discomfort. After examination, however, Dr. Massaro-Giordano found no obvious signs on her corneal surfaces either, leading her to again suspect a neurogenic etiology—more specifically, trigeminal dysphoria.
As with the first case, Dr. Massaro-Giordano treated the patient with anti-inflammatory eye drops and autologous serum drops. In addition, she referred the patient to an optometrist who regularly checks patients for ocular strain and misalignments. The exam revealed a mild misalignment and the patient’s symptoms improved when she was fitted with specialized contoured prism glasses.
“The trigeminal nerve that senses eye pain, evaporation, discomfort, and dryness will also sense discomfort if your eyes are not working together well.”
“What’s happening is that the trigeminal nerve that senses eye pain, evaporation, discomfort, and dryness will also sense discomfort if your eyes are not working together well,” Dr. Massaro-Giordano says. Even subtle misalignments can strain the brain’s ability to correctly fuse the two images, she says, which the trigeminal nerve expresses as dryness.
By helping to resolve that misalignment, the specialized glasses can alleviate that strain and improve the dryness sensation. “It’s not all about the clarity of vision, but it’s about the comfort of vision as well,” she says.
A Closer Look at Corneal Nerves
To further aid her efforts in identifying the true source of pain for her patients, Dr. Massaro-Giordano is using the CellChek C® wide-field scanning specular microscope to detect subtle differences in corneal nerve morphology. NYU Langone was the first institution in North America to acquire the state-of-the-art microscope, which is currently being used for research purposes only.
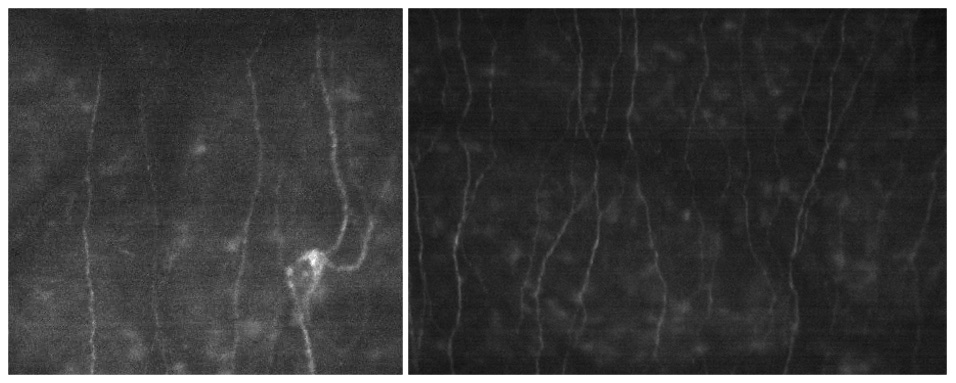
Currently, Dr. Massaro-Giordano is comparing images from patients with dry eye disease to those from healthy controls. “We’re looking for specific changes in the nerves: Are they diminished, trying to regenerate, or inflamed? Are there microneuromas?” she explains.
So far, her analysis suggests that patients with ocular misalignments have relatively normal-appearing nerves. By contrast, patients with pronounced nerve pain symptoms have nerves that appear more inflamed, diminished, or abnormal. “These can give us clues as to which direction we need to go,” she says.