Referral Notes:
- The EFP neurofeedback technology, Prism, has shown a 32 percent remission rate and a 67 percent response rate in PTSD.
- NYU Langone was the only U.S. site to participate in the pivotal trial supporting FDA clearance and now offers it to patients with PTSD and depression.
- NYU Langone researchers have also studied Prism in ADHD, are participating in a large-scale trial comparing Prism with sham treatment in adults with PTSD, and have launched a study in adolescents with PTSD.
Psychotherapeutic and pharmacologic therapies are designated as first-line treatments for post-traumatic stress disorder (PTSD), but both approaches have considerable shortcomings. Only 30 to 60 percent of patients who undergo psychotherapy for PTSD achieve remission, and many drop out due to the necessity of re-experiencing their trauma. Attrition rates are also high for the most-prescribed medications, including antidepressants and atypical antipsychotics, owing to their limited effectiveness and unwanted side effects.
A novel interventional technology, amygdala-derived EEG-fMRI-pattern (EFP) neurofeedback, offers a promising adjunct to traditional therapies for PTSD. Emerging research suggests that it can enhance the efficacy and tolerability of those methods—or even provide an alternative for patients who are unwilling or unable to receive them. The first device based on the EFP approach, Prism, was granted FDA clearance in 2023 based on an international clinical trial for which NYU Langone Health served as the sole U.S. site.
“Interventional techniques like neurofeedback may prove as transformative as interventional cardiology has been for cardiac care.”
Charles R. Marmar, MD
NYU Langone researchers continue to pioneer EFP neurofeedback, exploring its utility not only in PTSD, but also in other disorders. “By directly targeting the brain circuitry underlying neuropsychiatric illness, interventional techniques like neurofeedback, transcranial stimulation, and deep brain stimulation may prove as transformative as interventional cardiology has been for cardiac care,” says Charles R. Marmar, MD, the Peter H. Schub Professor and Chair in the Department of Psychiatry.
A Video Game that Targets Dysfunctional Brain Circuitry
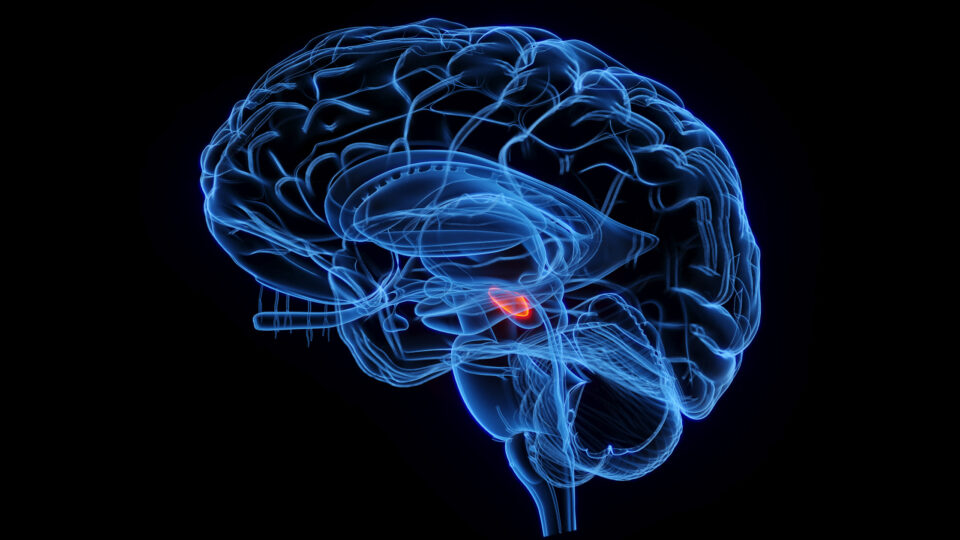
Neurofeedback uses real-time representations of brain activity to train patients to regulate hyperactive neural circuits. The idea of employing it to target the amygdala in PTSD dates to the 1990s, when that structure’s key role in mediating the disorder was first recognized. Early efforts relied on electroencephalography (EEG), whose poor spatial resolution brought inconsistent results.
More recently, fMRI-based neurofeedback for PTSD has shown efficacy in experimental settings. However, the disadvantages of fMRI include high expense, low accessibility, and the stress patients often experience when enclosed in a cramped, noisy scanner.
EFP neurofeedback combines the anatomical precision of fMRI and the convenience of EEG, while avoiding the downsides of both imaging methods. The method was developed by Israeli researchers, who began by taking EEG scans while study subjects performed fMRI-based neurofeedback training. The EEG readings were then analyzed by machine learning algorithms to detect an “electronic fingerprint,” or EFP, associated with amygdala BOLD (blood oxygenation level dependent) signals from the fMRI. The team used this data to create an EEG-based neurofeedback program.
This model became the basis for the Prism system. Patients with PTSD wear an EEG cap while playing a video game in which a crowd of avatars mills about an airport waiting area. The goal is to make them return to their seats—a task that requires users to downregulate their amygdala activity. During each 15-minute session, the Prism program assesses the patient’s EFP, detects when the amygdala is being actively downregulated, and translates that to the action on the screen.
“This is one of the first treatments in which patients with PTSD don’t have to take a pill or talk about their trauma in detail, which is very painful for some people,” Dr. Marmar notes.
Early Research Shows Encouraging Results
In the open-label trial that led to FDA clearance, 79 patients with PTSD underwent 15 Prism sessions over an eight-week period. All participants continued with psychotherapy or medication throughout the study, including a cohort of treatment-resistant combat veterans with chronic PTSD.
After completing treatment, 32 percent of participants achieved remission, and 67 percent met the criteria for a clinically significant reduction in Clinician Administered PTSD Scale for DSM-5 (CAPS-5) scores. At three-month follow-up, the average reduction in CAPS-5 total scores was a robust 13.5 points.
Significant improvements were also seen in other validated measures of PTSD as well as depression. Adverse events were mild and transient, and the dropout rate was low.
“We think [EFP neurofeedback] offers significant potential not only for treating PTSD, but also for other disorders in which amygdala dysfunction plays an important role,”
Lenard A. Adler, MD
“We think this approach offers significant potential not only for treating PTSD, but also for other disorders in which amygdala dysfunction plays an important role, such as depression and attention deficit hyperactivity disorder,” says Lenard A. Adler, MD, director of NYU Langone’s Adult ADHD Program. “It’s affordable and scalable. And because it can be delivered by trained technicians, it could increase access to effective therapy in areas where psychiatrists are in short supply.”
New Studies Aim to Unlock Prism’s Potential
At NYU Langone, Prism is available to all patients with PTSD, as well as those with treatment-resistant depression. “We’re hearing encouraging reports from both groups,” says Dr. Marmar, “but we don’t have rigorous data on outcomes yet.”
To gain deeper insights on Prism’s effectiveness and its suitability for different patient populations, NYU Langone researchers are conducting further investigations. A 2024 pilot study, for example, led by Drs. Adler and Marmar, found that Prism reduced ADHD symptoms in adults.
The team is currently recruiting for a multisite study, funded by the Department of Defense, of adjunctive Prism versus sham treatment for PTSD in U.S. veterans and civilians. Pediatric neuropsychologist Richard Gallagher, PhD, also recently launched a pilot study of Prism in adolescents with PTSD.
“If the research holds up, this technique could become a crucial tool in our toolbox,” says Dr. Marmar. “We’re very excited about that possibility.”