Referral Notes:
- How thoughts translate into actions is key to understanding the pathophysiology of Parkinson’s and other movement disorders.
- NYU Langone researchers are shedding new light on neural pathways linking cognitive and movement decisions in the basal ganglia and motor thalamus.
- Decoding these underlying mechanisms could enable improved approaches to deep brain stimulation for a wide range of neuropsychiatric conditions.
Among the central questions in neuroscience is how thoughts translate into actions—and how that process goes awry in movement disorders. A healthy person, for example, can turn around the instant she realizes she left her keys in her car. A patient with Parkinson’s disease, by contrast, may find it difficult to spontaneously change course. However, the “glue” that binds cognitive and motor processes is poorly understood.
Dennis London, MD, a neurosurgeon at NYU Langone Health, is working to help solve this mystery, with a series of studies tracing how key nodes in the cortico-striatal-thalamic circuit govern motor planning and execution.
“Whether we’re treating Parkinson’s with medications or with surgery, we don’t know how to do anything about its cognitive symptoms, such as slowed thinking, planning difficulties, and deficits in executive function,” he explains. “And many of the things we do to treat the disease’s motor symptoms, like deep brain stimulation, can make the cognitive dysfunction worse.”
“Whether we’re treating Parkinson’s with medications or with surgery, we don’t know how to do anything about its cognitive symptoms.”
Dennis London, MD
He recently received NIH funding for the latest phase of his research, which could eventually result in better treatments not only for Parkinson’s, but also for conditions ranging from Tourette’s syndrome to schizophrenia. The project is a collaboration with neuroscientist Roozbeh Kiani, MD, PhD, and neurosurgeon Alon Mogilner, MD, PhD.
“There’s an interplay between movement disorders and cognitive disorders related to this circuit,” Dr. London explains. “The hope is that learning how it works will enable us to develop interventions in a more targeted manner.”
Surprising Findings from a First-in-Human Trial
To dissect the neural mechanisms underlying changes in motor plans, Dr. London has focused on the subthalamic nucleus (STN)—an inhibitory node in the basal ganglia, which plays crucial roles in both movement and cognition, and a common target for deep brain stimulation (DBS).
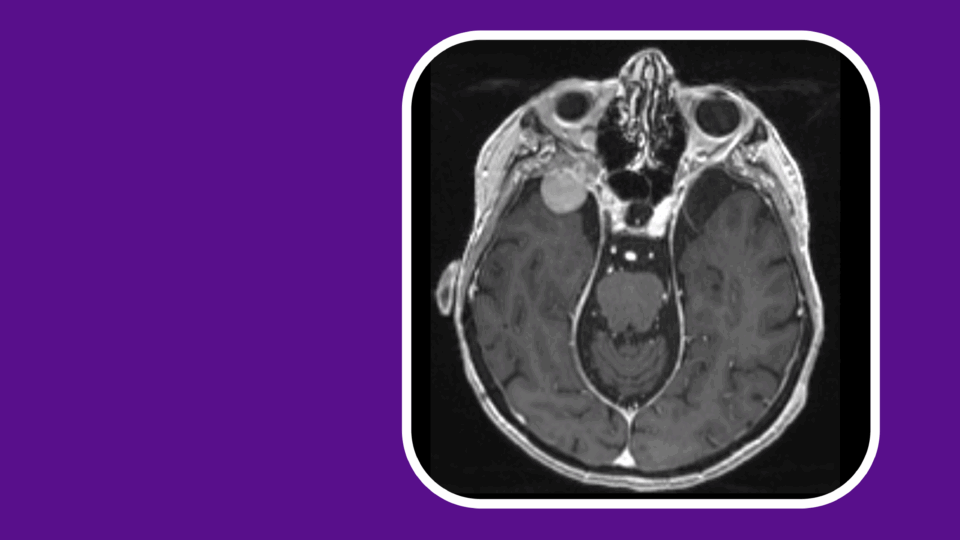
In the first in-human trial of its kind, Dr. London and colleagues examined STN neural activity during planned and unplanned changes of movement. They developed a behavioral task in which participants with Parkinson’s disease undergoing implantation of DBS electrodes moved their hands on a straight or turning trajectory. On a random subset of trials, participants were told to initiate a straight reach but then unexpectedly cued to switch to a turning trajectory mid-movement.
The results, published in eLife in 2021, were striking. Overall STN activity decreased during switches, with further analysis revealing a complex response: distinct clusters of neurons encode the movement plan, hand kinematics during the movement, and changes in the movement plan.
“The behaviors of these neurons may reflect their moment-by-moment degree of confidence that a recently planned movement will be completed,” Dr. London says.
“Our goal is to use the insights from this research to develop stimulation strategies that treat movement and cognitive deficits in neuropsychiatric disorders as two sides of the same coin.”
These findings could provide clues on how to optimize delivery of DBS to benefit movement decisions in Parkinson’s while minimizing cognitive impact. The results also call into question established theories that the STN contributes to switching an action plan by increasing its activity to halt the initial action. “Our findings suggest that the STN plays a very different role from what previous theories postulated,” Dr. London says.
Addressing Both Sides of the Therapeutic Coin
Dr. London’s new study builds on this work by looking beyond the STN—and beyond Parkinson’s. He and his colleagues are examining the effects of movement-plan changes in other nodes in the cortico-striatal-thalamic circuit: the globus pallidus, another common target for DBS in Parkinson’s disease, and the motor thalamus, the primary target for DBS in essential tremor.
“We want to see what’s happening throughout this circuit, and to learn whether similar mechanisms are operating in related disorders,” he explains.
In future research, Dr. London plans to investigate whether dysfunctions in these mechanisms can be corrected using specially calibrated approaches to DBS. Such approaches, he suggests, could also provide alternatives to antidopaminergic medications for conditions such as schizophrenia, whose side effects include movement disorders.
“Our goal,” he says, “is to use the insights from this research to develop stimulation strategies that treat movement and cognitive deficits in neuropsychiatric disorders as two sides of the same coin.”