Histotripsy, first developed two decades ago, has emerged as a groundbreaking tissue ablation technology with diverse potential applications, from benign prostatic hyperplasia to cardiovascular disease and cancer treatment.
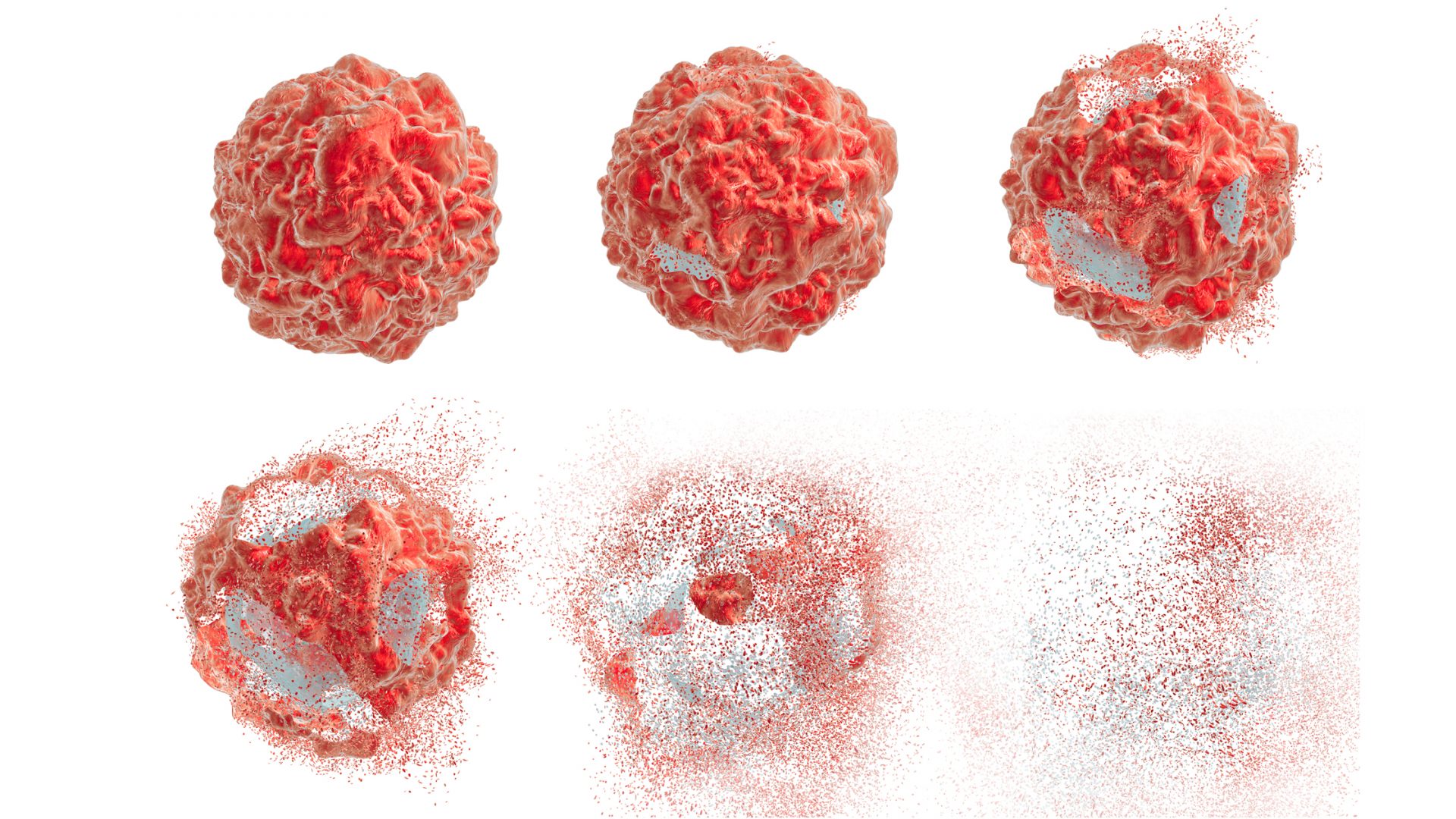
This noninvasive, non-ionizing, and non-thermal ablation method is guided by real-time imaging. Using short pulses of focused ultrasound, it mechanically destroys tissue through cavitation. A cloud of rapidly oscillating microbubbles pulverizes the target into acellular debris, which is eventually reabsorbed into the body.
In a milestone decision in October 2023, the FDA approved the first clinical use of histotripsy for the treatment of primary and metastatic liver tumors. NYU Langone Health’s Perlmutter Cancer Center is the first facility in New York City to offer the technique, which has several advantages over previous methods.
“Histotripsy enables us to treat patients who are ineligible for surgery and who would not generally be candidates for ablation.”
Brock Hewitt, MD, MPH
Unlike surgical ablation, histotripsy causes no bleeding, and minimal pain or scarring. It eliminates the “heat-sink” effect that limits thermal techniques near delicate structures such as bile ducts or blood vessels. Precision is further enhanced by dose-related tissue selectivity, and by continuous monitoring via ultrasound.
“Histotripsy enables us to treat patients who are ineligible for surgery and who would not generally be candidates for ablation because their tumors are in locations that are unsafe to target with thermal techniques,” says surgical oncologist Brock Hewitt, MD, MPH, who co-leads the histotripsy team at Perlmutter with interventional radiologist Mikhail Silk, MD. “This method has the potential to be first-line therapy for smaller tumors in the liver, though clinical trials for that application have not yet begun.”
A Surprising Immunological Effect
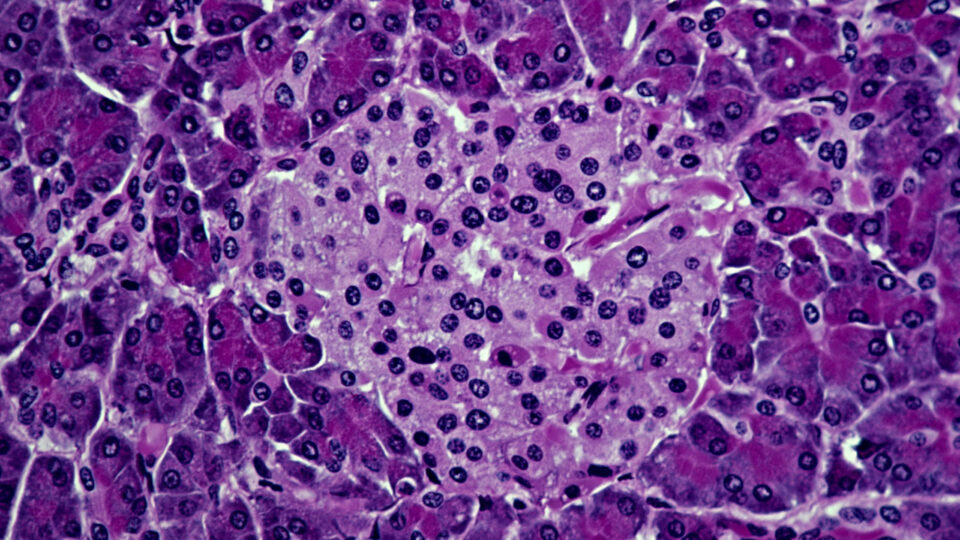
The FDA’s approval of histotripsy was informed by the multicenter, international #HOPE4LIVER trial, with a primary endpoint of technical success within 36 hours of treatment. The study found a primary efficacy of 95.5 percent in the 44 tumors treated, with a complication rate of 6.8 percent (comparable to other focal liver therapies). Results at six-month follow-up are expected to be published soon.
Evidence suggests the technique can also have a more surprising effect: training the immune system to destroy tumors elsewhere in the liver, by revealing antigens normally hidden behind cancer cells’ outer membranes. This mechanism could also potentially prevent recurrence.
“Histotripsy has been shown to have abscopal effects in subjects with additional disease not targeted by the treatment.”
Mikhail Silk, MD
“In preclinical as well as clinical studies, histotripsy has been shown to have abscopal effects in subjects with additional disease not targeted by the treatment,” says Dr. Silk. “The data on these potential benefits is preliminary, but it provides a promising avenue for further research.”
A Precise, Streamlined Procedure
Hepatic histotripsy is delivered using a system that includes an imaging probe, a programming station, and a focused ultrasound transducer attached to a robotic arm.
At NYU Langone, treatment is administered in the interventional radiology suite. After the patient is placed under anesthesia and intubated, the team performs a diagnostic ultrasound. “If we can see the lesion, and it’s no larger than 4 centimeters, we can perform the procedure,” says Dr. Hewitt. “We can treat 50 to 60 percent of the liver, including areas behind the ribs.”
Once the target zone is visualized, the device is programmed to guide the transducer, working in increments of 3 to 6 millimeters. To minimize respiratory movement that could interfere with accuracy, patients receive jet ventilation. The bubble cloud acts as a natural contrast agent, allowing clinicians to calibrate and assess the treatment as they work.
“If we can see the lesion, and it’s no larger than 4 centimeters, we can perform the procedure.”
Dr. Hewitt
The procedure, which takes about two hours from start to finish, requires little recovery time. And because histotripsy enables the body to reabsorb the targeted tissue, rather than leaving a necrotized remnant, long-term complications are rare.
Improving Outcomes and the Patient Experience
These benefits help explain why NYU Langone became one of the first health systems in the nation to deploy the new technique.
“We have a longstanding commitment to leveraging innovative technology, and we’re fortunate to have the institutional resources to make that possible,” says Dr. Hewitt, who also leads Perlmutter’s robotic pancreatic surgery program—the highest-volume practice of its kind in the city. “Our adoption of histotripsy reflects our central mission: to improve outcomes, and to optimize the overall experience for the patient.”