Referral Notes:
- The Platelet Reactivity ExpresSion Score (PRESS) is the first tool to assess platelet reactivity using genetic signatures.
- In one study to validate the tool, PRESS was higher in women who had a heart attack than those with stable heart disease.
- In another study, patients with atherosclerosis and a PRESS above the median were 90 percent more likely to experience a major cardiovascular event.
- The PRESS tool could enable more personalized treatment decisions, such as prescribing anti-platelet therapies like aspirin, based on individual platelet function.
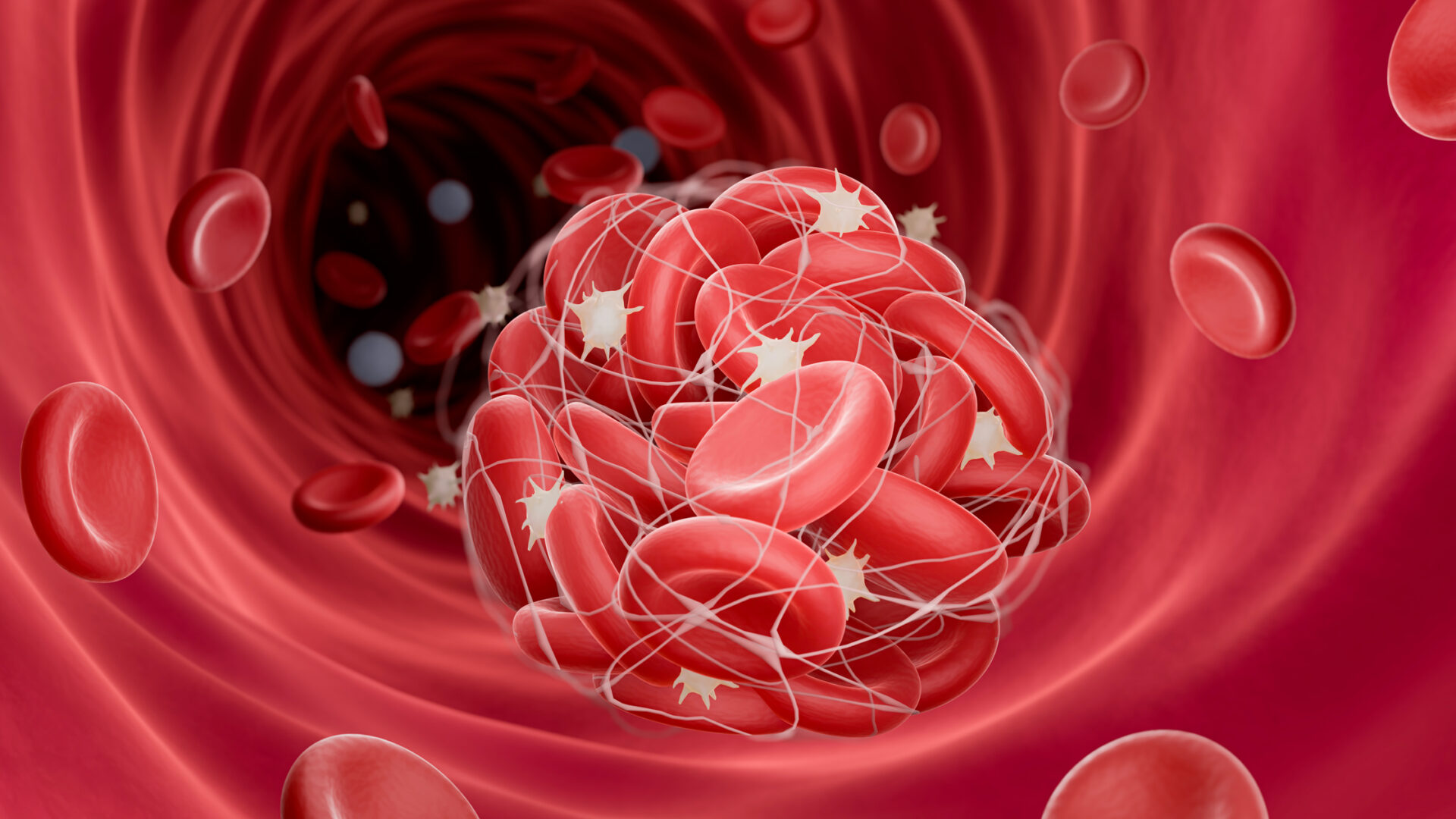
Cardiologists have long known that increased platelet reactivity is a risk factor for cardiovascular events, yet limited tools exist to identify individuals with a hyperreactive platelet phenotype. In a study recently published in Nature Communications, researchers at NYU Langone Health developed the first transcriptome-based test designed to do just that.
The tool, dubbed the Platelet Reactivity ExpresSion Score (PRESS), uses the genetic signature of a patient’s platelets to assess reactivity, making it far more precise and less labor-intensive than conventional aggregometry techniques.
“Our results demonstrate that this scoring system can circumvent aggregometry or other platelet activity measurements to reliably predict platelet hyperreactivity and the related risk of cardiovascular events,” says lead author Jeffrey S. Berger, MD, director of the Center for the Prevention of Cardiovascular Disease. “It can be used successfully across populations, both in patients at risk of heart attacks and in healthy people whose future risk would otherwise remain unknown.”
Aggregometry Challenges
Although aggregometry is commonly used to detect insufficiently reactive (dysfunctional) platelets, routine measurement of platelet hyperreactivity has been infeasible to date. Aggregometry tests were not originally designed for that purpose, and until recently they lacked the sensitivity to determine how much reactivity was too much.
Over the past decade, the field has shifted toward a more calibrated method: exposing platelets to a tiny dose of epinephrine, which weakly encourages aggregation. Experts have settled on 60 percent aggregation in a platelet sample at 0.4 μM (micromoles) of epinephrine as the threshold over which platelets are designated as hyperreactive.
Still, the correlation between this metric and cardiovascular events remains uncertain—and a standard clinical test for platelet hyperreactivity remains elusive. Both deficiencies persist, in part, because results delivered by even the most sophisticated aggregometry techniques often vary from lab to lab.
“This scoring system can circumvent aggregometry to reliably predict platelet hyperreactivity and the related risk of cardiovascular events”
Jeffrey S. Berger, MD
To overcome the latter obstacle, a team led by Dr. Berger and Tessa J. Barrett, PhD, conceived of a “liquid biopsy”—a test based on the platelets’ gene expression. “We thought this approach would be more reproducible than subjecting platelets to chemical exposure in a test tube,” Dr. Barrett explains.
Test Validation
In the current study, Dr. Berger’s team set out to answer three questions: whether patients whose platelets met the existing definition for hyperreactivity were, in fact, at greater risk for cardiovascular events; whether their platelets’ genetic signature could be used as a biomarker of hyperreactivity; and whether the patients’ degree of cardiovascular risk could be assessed using such a marker.
The researchers began by using epinephrine-induced aggregometry to track the impact of platelet activity status on major adverse cardiovascular and limb events (MACLE) in patients with peripheral artery disease. MACLE was measured in this group of high-risk patients after they underwent lower extremity revascularization.
Among 254 participants whose platelet aggregation was measured with 0.4 μM of epinephrine, 17.5 percent showed hyperreactive platelets. That cohort, the team found, had more than double the incidence of MACLE within 30 days after lower extremity revascularization than patients without hyperreactivity.
Next, the team used RNA sequencing to search for genetic differences associated with hyperreactivity in platelet material collected from 129 of the patients. They found that 451 transcripts were significantly correlated with percent aggregation to epinephrine. The researchers designed the PRESS scoring system based on these results, then confirmed its accuracy by checking it against platelet aggregation tests.
To further validate PRESS, the team explored the link between the score and cardiovascular risk in other patient groups. Among these was the Heart Attack Research Program, which enrolled women undergoing coronary angiography. In this group, PRESS was found to be higher in those who had a heart attack than in those with stable coronary artery disease. Among patients with lower extremity atherosclerosis followed for an average of 18 months, patients with PRESS above the median score were 90 percent more likely to have a major cardiovascular event than those below it.
PRESS Forward
Besides providing a potentially transformative method for assessing thrombosis-related cardiovascular risk, the PRESS test could help patients and physicians make better-informed decisions on treatment. One example is the question of whether an individual should take aspirin, which counters clotting but increases the risk of bleeding.
“Our score has the potential to personalize cardiovascular disease risk prevention.”
Tessa J. Barrett, PhD
“Physicians currently prescribe this medication based on available risk factors, including high cholesterol or high blood pressure, which are not directly related to platelet function,” says Dr. Berger. “PRESS promises to help physicians tailor antiplatelet treatment to the people most likely to benefit: those with platelet hyperreactivity.”
“A platelet-based test would help us optimize therapeutic approaches to fit each patient’s needs,” adds Dr. Barrett. “Our score has the potential to personalize cardiovascular disease risk prevention.”