As 2026 marks the 20th anniversary of the NYU Langone Orthopedic Hospital—a merger of the Hospital for Joint Diseases and NYU Langone Health—Joseph D. Zuckerman, MD, chair of orthopedic surgery, reflects on the merger and his decades of leadership. Here, he highlights the pivotal decisions and values that transformed a specialty hospital into the No. 2 orthopedic program in the country, per U.S News & World Report.
Physician Focus: Your vision was to build a “major orthopedic department at a major academic medical center,” not another specialty hospital. How has that vision shaped your strategy?
Dr. Zuckerman: That distinction has been fundamental. Back in 1997, when I became department chair, there were other orthopedic hospitals in the country—but I didn’t want to be known as one. I wanted our excellence reinforced by an integrated academic medical center, reinforcing other specialties in return.
“When I became department chair, there were other orthopedic hospitals in the country—but I didn’t want to be known as one. I wanted our excellence reinforced by an integrated academic medical center.”
Joseph D. Zuckerman, MD
That vision drove our full 2006 merger, when the excellence in care offered by the Hospital for Joint Diseases became backed by the infrastructure of NYU Langone. With support from leadership, we rapidly integrated operations and scaled data-driven quality initiatives.
Later, when we acquired hospitals in Brooklyn and on Long Island, we never viewed them as separate facilities. We integrated everything: standards, data systems, quality protocols. That “systemness” is what continues to set us apart from orthopedic specialty hospitals operating in silos.
Physician Focus: How has the NYU Langone Orthopedic Center changed the delivery of outpatient orthopedic care?
Dr. Zuckerman: Launched in 2013, the center is far more than a one-stop shop. Previously, patients saw an orthopedist, then were sent to another specialty, such as rheumatology, on another day, or to another location for an MRI, then to physical therapy elsewhere—a fragmented, inefficient approach. At our center, all services happen in one location on the same day, with specialists communicating and adjusting care in real time.
“The most meaningful innovation is in bringing our core principles to scale: multidisciplinary collaboration, integrated workflows, and shared accountability for outcomes.”
The most meaningful innovation is in bringing our core principles to scale: multidisciplinary collaboration, integrated workflows, and shared accountability for outcomes. Whether you’re in Manhattan or Brooklyn or on Long Island, we follow the principle of “one department, one standard,” regardless of where you receive your orthopedic care.
Physician Focus: With over 200 orthopedic surgeons across multiple sites, how do you sustain quality at scale?
Dr. Zuckerman: Data and transparency. We review all quality metrics on a monthly basis at minimum. Every division—adult reconstruction, sports medicine, trauma, spine surgery, pediatrics, and others. And each location participates and is accountable for their metrics.
When the 30-day readmission rate at NYU Langone Hospital—Brooklyn was found to be higher than expected—and above our target—our site chief analyzed every case. A pattern emerged: blood thinner protocols to prevent thromboembolism designed for hip and knee replacement weren’t optimal for spine surgery. In response, we adjusted our deep vein thrombosis prevention protocol to prevent the readmissions.
“Attention to that level of detail drives real improvement.”
We also track physician communication scores against our 90th percentile target. Anyone below gets support: peer review, rounding with colleagues, patient observation. Attention to that level of detail drives real improvement.
Physician Focus: As the nation’s largest orthopedic residency program—now expanding from 14 to 16 residents per year—how do you prepare future leaders?
Dr. Zuckerman: As many universities advertise, we aim for a “big school with a small-school feel.” We’re the largest program, but our dedicated residency program directors and integrated weekly didactic conferences help keep us cohesive. In addition, our residents work in teams while developing relationships across the entire residency program.
Beyond training, we’re deeply committed to diversity. Over a third of those in our program are women, with meaningful representation of underrepresented minorities—well above the orthopedic specialty average. We run pipeline programs to support underrepresented groups and annually host over 100 fourth-year medical students from around the country for audition rotations. If we’re training the next generation of orthopedic leaders, they need to reflect the communities we serve.
Physician Focus: What are your priorities for the next phase of growth?
Dr. Zuckerman: First, accessibility and patient experience—streamlining every detail from first contact through last visit, and scaling resources so patients can be seen sooner.
“Ninety percent of what we do should be standardized across the system, with just 10 percent individual variation allowed for each unique situation.”
Second, what I call the 90/10 rule: 90 percent of what we do should be standardized across the system, with just 10 percent individual variation allowed for each unique situation. This ensures consistency in patient care while respecting clinical judgment.
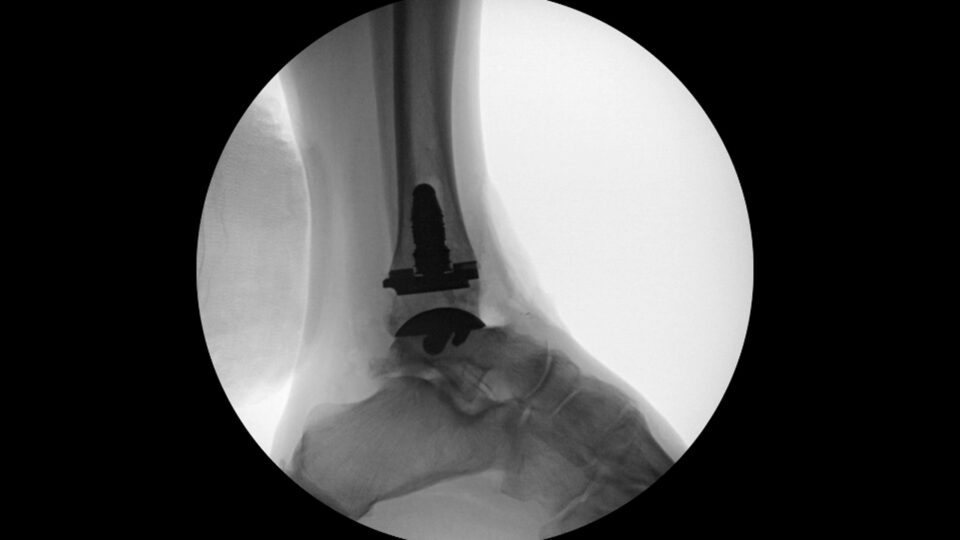
Third, we’re advancing minimally invasive and robotic surgery, expanding stem cell and cartilage work, and leveraging our prolific research—we publish over 300 peer-reviewed articles annually. Innovation rooted in clinical outcomes is how we will continue to shape national standards.