Referral Notes:
- Bronchoscopic cryoimmunotherapy (BCI) presents a novel approach that aims to augment the immune response against lung tumors.
- A first-in-human phase 1 clinical trial investigating BCI in advanced NSCLC demonstrated promising safety and feasibility and provides preliminary evidence of immune activation.
- Larger prospective studies are needed to explore BCI’s potential synergistic effects with existing treatment modalities.
Bronchoscopic cryoimmunotherapy (BCI) delivered during standard-of-care bronchoscopy may be safe and feasible among patients with advanced non-small cell lung cancer (NSCLC), according to research published in JTO Clinical and Research Reports.
Of 95 patients with documented or suspected advanced stage 2B/3/4 NSCLC who were screened at NYU Langone Health between January 2020 and March 2024, BCI was successfully performed in 21 patients, achieving 100 percent feasibility, one of the primary end points of this first-in-human, phase 1 dose-escalation trial.
Before receiving BCI, all patients were scheduled to undergo a standard-of-care bronchoscopy for diagnostic and/or staging purposes.
“The goal of this treatment is not to simply destroy tissue, but instead to leverage it for the purpose of generating antitumor immune responses.”
Daniel H. Sterman, MD
“The goal of this treatment is not to simply destroy tissue, but instead to leverage it for the purpose of generating antitumor immune responses,” says study senior author Daniel H. Sterman, MD, the Thomas and Suzanne Murphy Professor of Pulmonary and Critical Care Medicine.
Cryoimmunotherapy: A New Frontier in Cancer Treatment
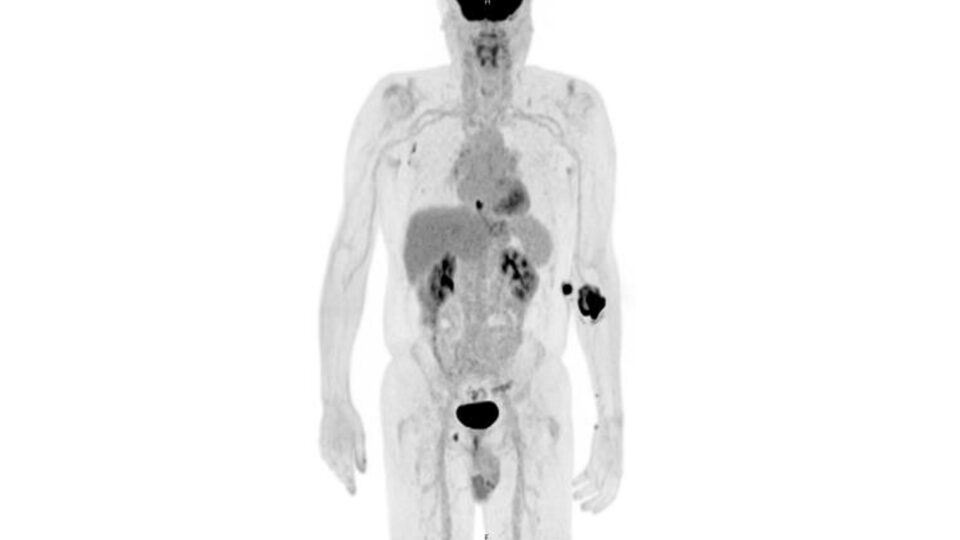
Combining cryoablation and immunotherapy presents a promising approach to generate potent systemic antitumor responses to peripheral lung cancers, with the potential to enable responses in patients who are refractory to immune checkpoint inhibitors (ICIs).
The technique leverages repetitive freeze-thaw cycles to elicit cell injury, thereby inducing necrosis and apoptosis of tumor tissue through the formation of intracellular ice crystals, cell dehydration, vascular compromise, and other mechanisms.
“Damaged tumor cells post-cryoablation release tumor neo-antigens, which are taken up by local dendritic cells, which then induce tumor-specific CD8+ T-cell activity,” explains Dr. Sterman.
First-In-Human, Dose Escalation Trial
In the study, researchers evaluated the safety and feasibility of BCI monotherapy in patients with advanced-stage NSCLC, and also explored whether BCI elicits antitumor immunologic responses in these patients.
BCI proved both safe and feasible—reaching a maximum dose (freeze time) of 30 seconds—with no patients experiencing dose-limiting toxicities or adverse events related to the procedure.
Additionally, the researchers observed preliminary evidence of immune modulation after BCI. Pre- and post-BCI peripheral blood analysis revealed a significant reduction in derived neutrophil-to-lymphocyte ratio (dLNR) in the high-dose BCI group compared to the low-dose BCI cohort.
They also observed increases in inflammatory cytokines following BCI, including GM-CSF, IFN-γ, IL-1β, IL-17A, IL-2, and effector memory T cells.
“Our results provide an initial glimpse into the exciting future of bronchoscopic cryoimmunotherapy.”
“Our findings support the hypothesis that BCI may elicit antitumor immunologic responses in advanced NSCLC,” says Dr. Sterman. “Although we demonstrated that a freeze time of up to 30 seconds is safe, we have yet to establish a maximally tolerated or effective dose.”
Therapeutic Potential of BCI
According to Dr. Sterman, these findings lay the groundwork for future investigations aimed at characterizing the therapeutic potential of BCI as an adjunctive therapy in NSCLC.
“Our results provide an initial glimpse into the exciting future of bronchoscopic cryoimmunotherapy,” Dr. Sterman says. “BCI may have synergistic effects with existing treatment modalities.”
With ongoing advancements, the research team believes that BCI holds promise to improve outcomes for patients with advanced NSCLC, but larger prospective studies are needed.
“My prediction is that within five years, numerous phase 3 trials will be underway, and in 10 years, we will have established treatment pathways for cryoimmunotherapy-based approaches.”