Case Highlights:
- A single chest incision enabled access for complete tumor resection.
- Risks to the recurrent laryngeal nerve and brachiocephalic vein were minimized with extensive preoperative planning and intraoperative nerve monitoring.
- Elevated alpha-fetoprotein (AFP) suggested malignancy but pathology confirmed a benign teratoma, sparing chemotherapy and fertility.
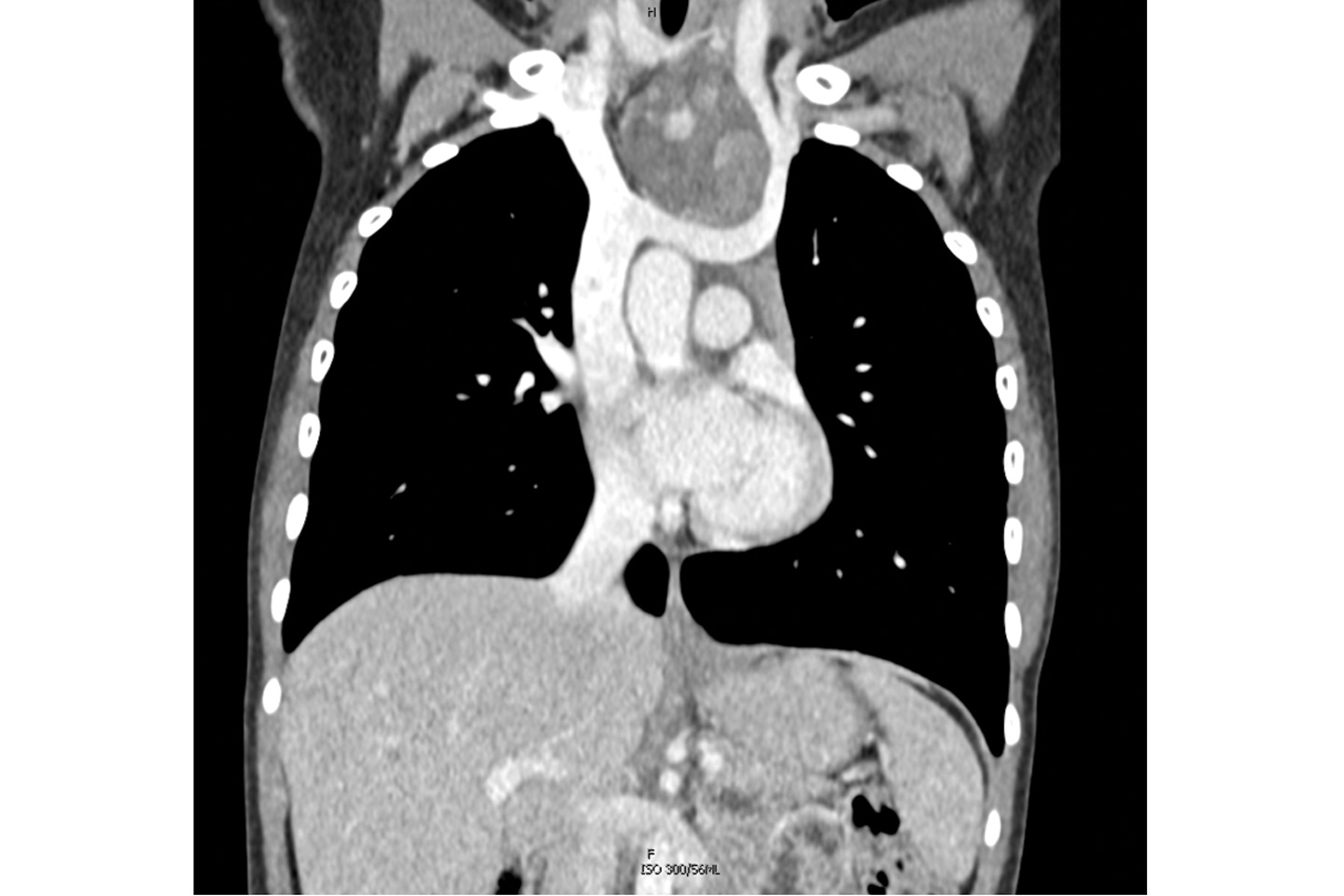
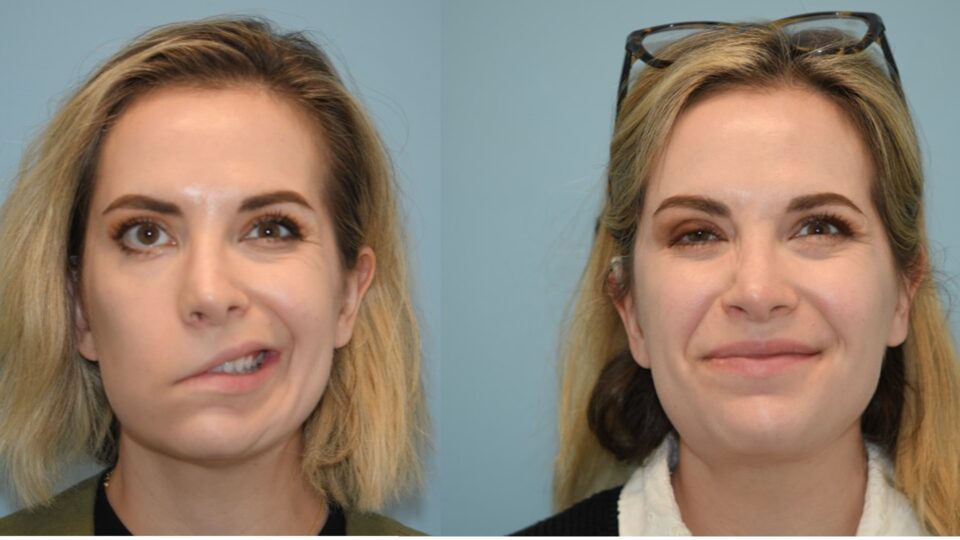
In the spring of 2025, an adolescent female was referred to NYU Langone Health head and neck surgeon Umamaheswar Duvvuri, MD, PhD, for evaluation of an anterior mediastinal mass. The mass was visible by eye, and point-of-care ultrasound revealed it to be a tumor extending from the lower neck into the chest.
“It appeared to be adjacent to, but not directly coming from or invading, the thyroid gland,” Dr. Duvvuri says. “Though we couldn’t be certain until surgery.”
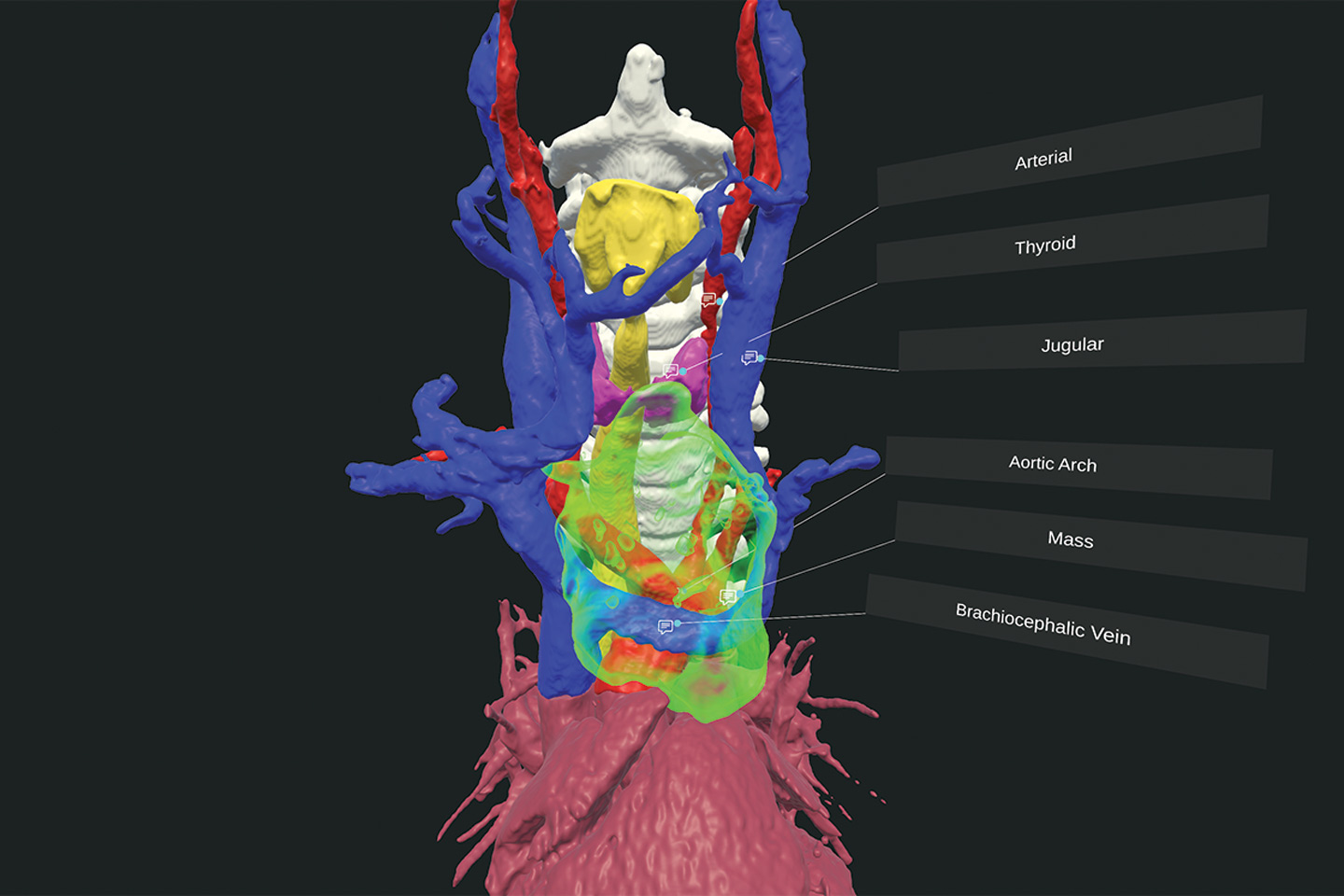
A biopsy confirmed a benign teratoma, but resection was expected to be complex; in addition to the tumor’s location spanning the neck and chest, and the concern for thyroid involvement, preoperative imaging revealed it to be in close proximity to the recurrent laryngeal nerve and possibly attached to the brachiocephalic vein.
“Speed is important, but ensuring the right environment and multidisciplinary team is paramount.”
Umamaheswar Duvvuri, MD, PhD
“The best time to treat any of these tumors is the first time,” Dr. Duvvuri says. “Speed is important, but ensuring the right environment and multidisciplinary team is paramount.”
Open Surgery Approach
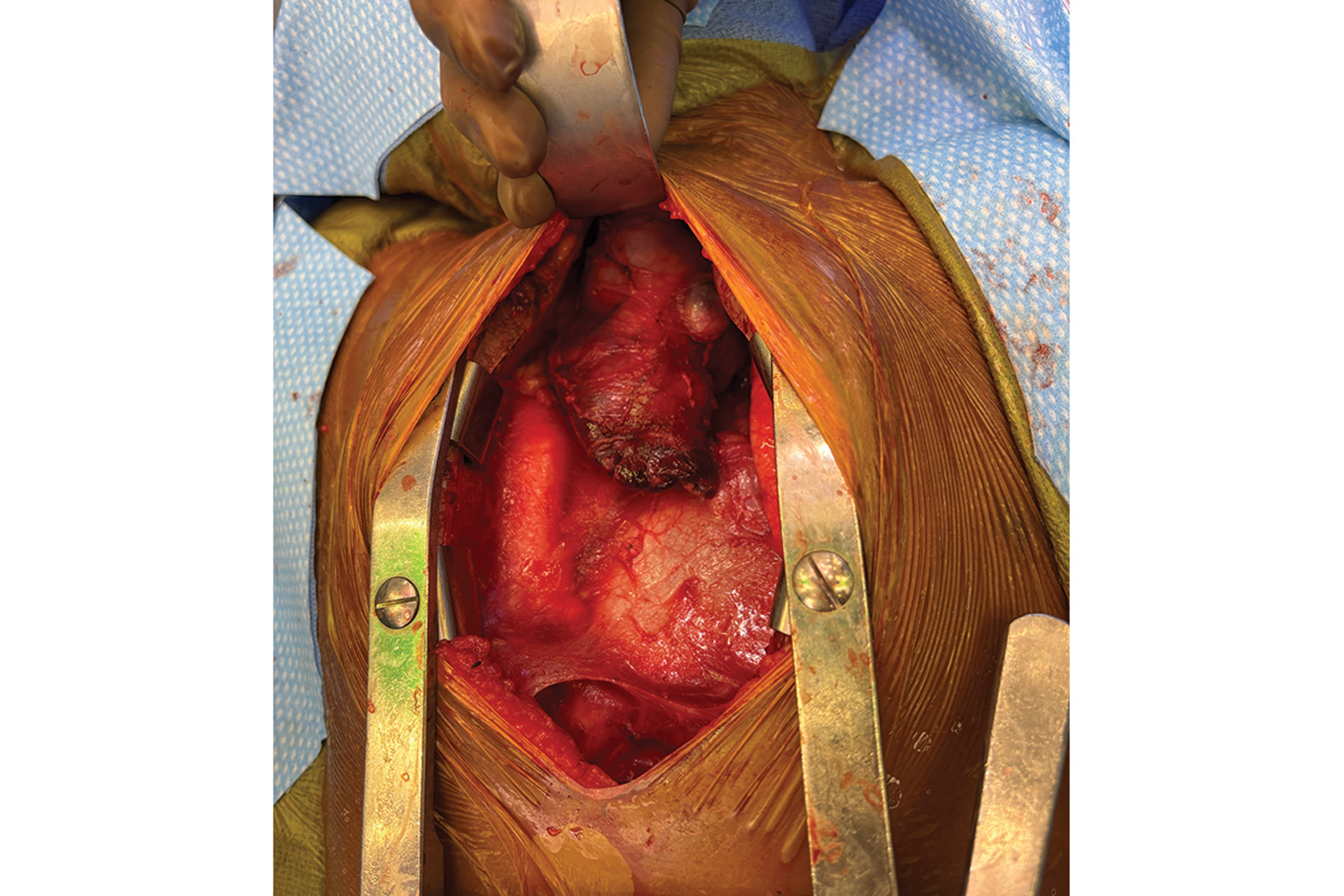
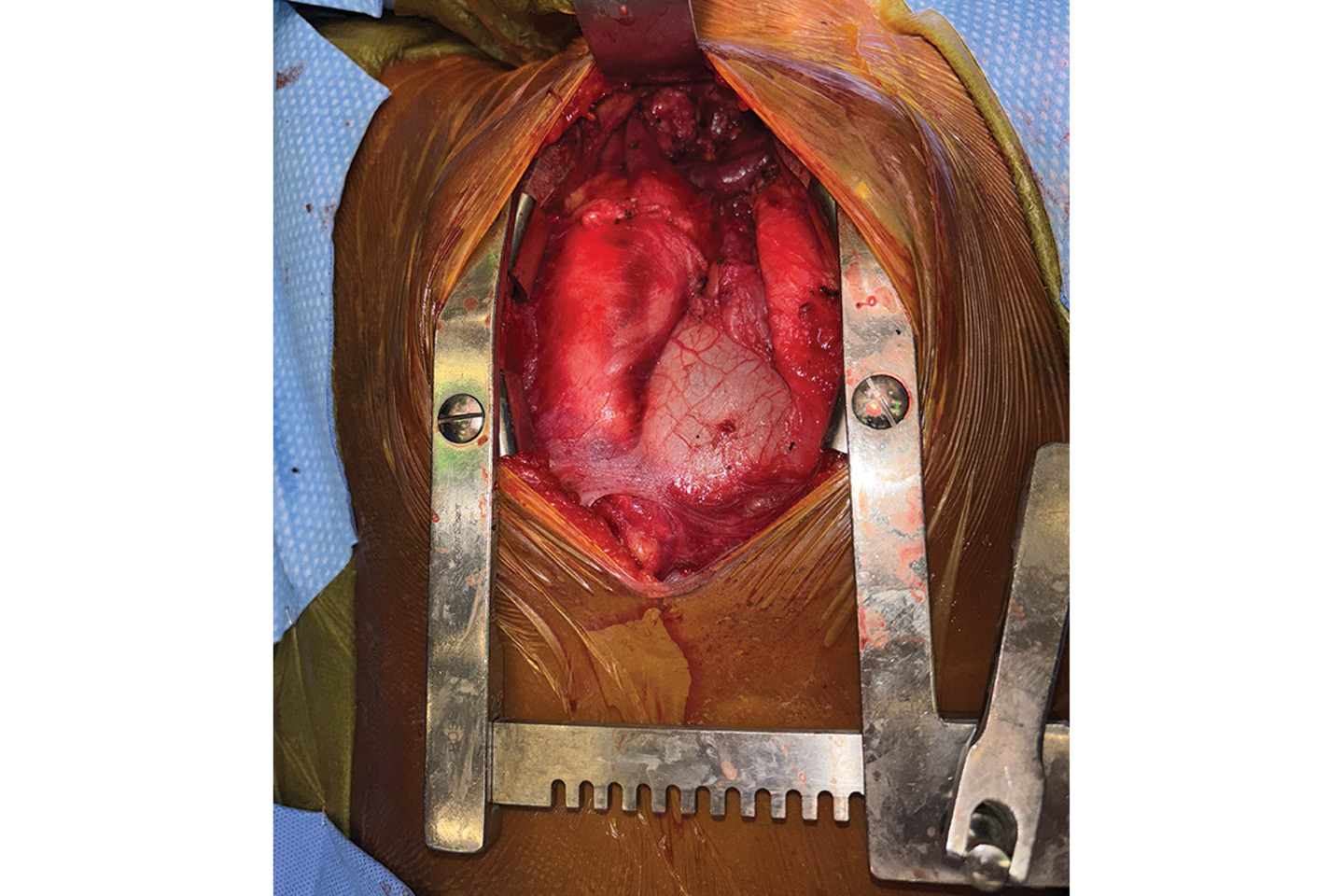
At a multidisciplinary tumor conference, a median sternotomy was chosen as the best operative approach. It would enable complete resection through a single chest incision and avoid the need for a separate incision at the neck. Jason C. Fisher, MD, a pediatric surgeon, and T.K. Susheel Kumar, MD, a congenital heart surgeon at Hassenfeld Children’s Hospital, prepared to address the cardiothoracic component.
While imaging revealed the tumor to be sitting just anterior to the brachiocephalic vein, it was uncertain whether the two would easily separate. “If the tumor and vein were attached, we were ready to place the patient on ECMO to resect and graft the vein,” Dr. Fisher says.
Preoperative planning was aided by advanced virtual reality visualization and the cardiac imaging expertise of Puneet Bhatla, MD. “We prepared for every scenario, from vascular reconstruction to emergency support, so that once the chest was open, we could proceed confidently and safely,” says Dr. Kumar.
“We prepared for every scenario, from vascular reconstruction to emergency support.”
T.K. Susheel Kumar, MD
To avoid injury to the recurrent laryngeal nerve, Dr. Duvvuri used intraoperative nerve monitoring. His team was also prepared to resect the thyroid if tumor invasion was found.
Intraoperatively, the best-case scenario emerged: no tumor attachment to the brachiocephalic vein or invasion into the thyroid. “But we were prepared for all of these eventualities,” Dr. Duvvuri says.
“We were able to provide complete tumor resection with the least morbidity and all of the emergency options available,” Dr. Fisher says. “That outcome underscores the strength of our children’s hospital and the expert collaboration among our disciplines.”
High AFP Posed an Early Challenge
After surgery, analysis of the resected tumor clarified an early diagnostic challenge.
While the biopsy—performed by interventional radiologist Frederic J. Bertino, MD—identified the mass to be a benign teratoma, initial bloodwork also revealed elevated levels of alpha-fetoprotein (AFP).
AFP, produced by the yolk sac and fetal liver during development, can indicate a malignant yolk sac tumor. Had this been confirmed on biopsy, neoadjuvant chemotherapy might have reduced the tumor size and simplified resection, but with potential harm to the patient’s fertility. Because the biopsy instead confirmed a benign teratoma, the team determined chemotherapy would be ineffective and unnecessarily risky.
“We were able to provide complete tumor resection with the least morbidity and all of the emergency options available.”
Jason C. Fisher, MD
Postoperative analysis then clarified the likely source of the AFP: the significant amount of liver tissue found within the teratoma. As germ cell tumors, teratomas can contain many different types of tissue, including liver.
Pediatric hematologist–oncologist Nicole Mallory, MD, and colleagues were critical in the decision to forgo chemotherapy, Dr. Fisher notes. “Our experienced pathology team confirmed that chemotherapy was unnecessary, sparing the patient both toxicity and fertility risks,” adds Dr. Duvvuri.
Recovery and Outlook
The patient’s recovery has been smooth and complication-free. “She’s doing very well,” Dr. Duvvuri says. “This is one of many recent cases in which our comprehensive head and neck program organized the best multidisciplinary care for a complex patient.”