Referral Notes:
- A pregnant patient at NYU Langone recently underwent successful meniscus and ACL surgery in her second trimester.
- The case followed the Division of Maternal–Fetal Medicine’s comprehensive protocol for non-obstetric surgery in pregnancy, developed in collaboration with inpatient obstetrics and obstetrics anesthesia.
- NYU Langone’s Sports Health program can refer pregnant patients to maternal–fetal medicine subspecialists for presurgical consultations.
Although non-obstetric surgery during a pregnancy can carry added risks if not handled adeptly, NYU Langone Health’s comprehensive and collaborative approach has given orthopedic patients far more options—and relief—than they often encounter elsewhere.
After being turned away from three other medical centers in the New York City region, a pregnant patient who had sustained an anterior cruciate ligament (ACL) tear and a displaced tear on her medial meniscus presented to NYU Langone in April 2025. Abigail L. Campbell, MD, director of the Center for Women’s Sports Medicine, concluded that although the woman’s ACL tear on its own didn’t require urgent surgery, her meniscus tear in that setting carried a high risk of worsening and becoming irreparable over time.
“Further, the location of her meniscus tear placed the knee at higher risk of instability, as the posterior horn of the medial meniscus provides a secondary stabilizer to anterior tibial translation,” Dr. Campbell explains. “When these are both torn, the chances of the knee giving out or buckling are significant at baseline. In pregnancy, with increased weight and ligament laxity, followed by the physical demands of carrying around a newborn, there is significant risk to the knee, the patient, and the baby.”
Coordination Through Sports Health
As director of the Division of Maternal–Fetal Medicine, Justin S. Brandt, MD, is well-versed in the downsides of delaying necessary non-obstetric surgeries in pregnant patients. During his residency, he published a case report on the potentially avoidable consequences of a delayed melanoma biopsy. “It’s not uncommon for providers to deviate from standard practice because someone is pregnant, and that’s a shame,” Dr. Brandt says.
“It’s not uncommon for providers to deviate from standard practice because someone is pregnant, and that’s a shame.”
Justin S. Brandt, MD
Through NYU Langone’s Sports Health program, which fosters cross-departmental communication and coordinates outreach to other providers as part of its integrated approach to patient health, Dr. Campbell connected with Dr. Brandt to discuss the case.
“I was impressed to learn that NYU Langone has an entire protocol for this exact indication: non-obstetric surgery in the pregnant patient,” she says. “By having access to other physicians within NYU Langone who are committed to the Sports Health mission, we were able to seamlessly provide the appropriate time-sensitive care for this woman.”
A Well-Considered Protocol
The surgical protocol, developed by maternal–fetal medicine in collaboration with inpatient obstetrics and obstetrics anesthesia specialists, has yielded evidence-based guidelines to maximize patient safety. Dr. Brandt met with Dr. Campbell’s patient as well to counsel her about the surgical planning, risks, and postoperative care and management.
“My job as a maternal–fetal medicine subspecialist is often to reassure patients that this is safe,” he says. “Yes, there are some risks, but if we delay the surgery, the risks may be greater and may even impact the patient’s long-term prognosis.”
Urgent surgeries, such as some cancer procedures, may be performed in the first trimester, but Dr. Brandt says the second trimester is best for most non-obstetric surgeries—past the first trimester and its increased risk for miscarriage but before the third trimester and its risk for preterm labor and delivery. “After 20 weeks of gestation, patients have to be positioned in a left lateral tilt position to avoid compression of the large blood vessels that supply blood to the heart,” he adds.
“If this had waited another few months, the meniscus tears would likely not have been able to be fixed.”
Abigail L. Campbell, MD
In some cases, intraoperative continuous fetal monitoring is conducted with capabilities to perform urgent cesarean deliveries, if necessary, though intermittent fetal assessment is preferred in most non-obstetric surgeries. Because pregnant patients are at higher risk for blood clots, early postoperative ambulation also is important, and some patients may receive blood thinners.
Despite the extra layer of complexity, Dr. Brandt says, thoughtful coordination by surgical and anesthesia teams to ensure good hemodynamics and perfusion can minimize the risk of obstetrical complications for most surgeries.
A Surgical Success
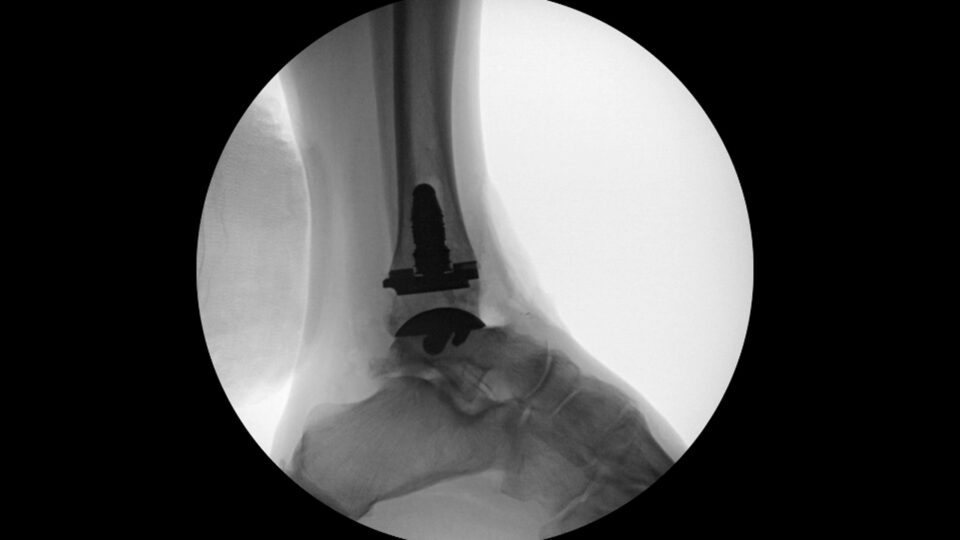
Dr. Campbell performed the meniscus and ACL surgery during the patient’s second trimester, during which the patient received a spinal anesthetic with sedation, followed by a postoperative nerve block for additional pain relief. “Most importantly, she had significant tearing in both medial and lateral menisci that were all reparable,” Dr. Campbell notes. “If this had waited another few months, the meniscus tears would likely not have been able to be fixed.”
The patient, now in her third trimester, has resumed low-impact cardiovascular exercise and light jogging, and recently went on a golf trip with her family. “She has excelled in her rehabilitation, is back to working in person, and is living a normal day-to-day life,” Dr. Campbell says.