By the time the patient, a woman in her late 60s, was referred to NYU Langone Health specialists Stella Chung, MD, and Douglas R. Lazzaro, MD, she had met with three ophthalmologists in the New York region over the course of several months.
Conjunctival erythema on the patient’s right upper eyelid, including the superior palpebral conjunctiva, diagnosed as a stye, wasn’t improving despite treatment with steroid eye drops, steroid injections, antibiotic ointment, warm compresses, and lid scrubs.
“It looked like blepharitis that had become chronic,” Dr. Chung says, “but diffuse redness of the globe, yellow eyelid changes, and lash loss across the entire central upper eyelid told me something was off. So, I performed a wide excisional biopsy.” Following excision of approximately one quarter of the upper eyelid for histopathologic evaluation and genetic testing, the correct diagnosis was confirmed as T2 sebaceous carcinoma of the eyelid.
“It looked like blepharitis that had become chronic, but diffuse redness of the globe, yellow eyelid changes, and lash loss across the entire central upper eyelid told me something was off.”
Stella Chung, MD
The potentially aggressive metastatic neoplasm of the oil glands is rare, representing approximately five percent of malignant eyelid tumors. “Sebaceous carcinoma of the eyelid is tested on our board exam every year, but many ophthalmologists will never see a single case in their entire career,” Dr. Chung says.
This was Dr. Chung’s first case in her seven years of oculoplastic practice, including training.
Surgical Approach
With a lesion of less than one centimeter, indicating early-stage disease, the patient didn’t require a sentinel lymph node biopsy. As the first step in treatment, NYU Langone Mohs micrographic and reconstructive surgeon Maressa C. Criscito, MD, performed Mohs surgery on the right eyelid to carefully excise the tumor while ensuring negative margins.
“Beware of the great masquerader of sebaceous carcinoma of the eyelid. It can look exactly like blepharitis or chalazion.”
The following month, Dr. Chung performed a Cutler-Beard flap, the two-stage gold-standard reconstruction technique for full-thickness defects spanning more than 50 percent of the upper eyelid. During the outpatient surgery, Dr. Chung created a bridge flap from the lower lid to replace the missing upper eyelid defect, with the tissue remaining pedicled to maintain its blood supply during the healing process.
The patient’s upper and lower lids remained sutured together for one month. After four weeks, once neovascularization occurred, Dr. Chung performed a second-stage division of the Cutler-Beard flap, separating the lids and reconstructing the lower eyelid margin.
Six months later, Dr. Chung performed a revision. “The patient’s lid wasn’t opposed on the globe as well as it should be. I tightened it and performed a blepharoplasty with skin graft from the other upper eyelid for a more natural appearance,” she says.
The Great Masquerader
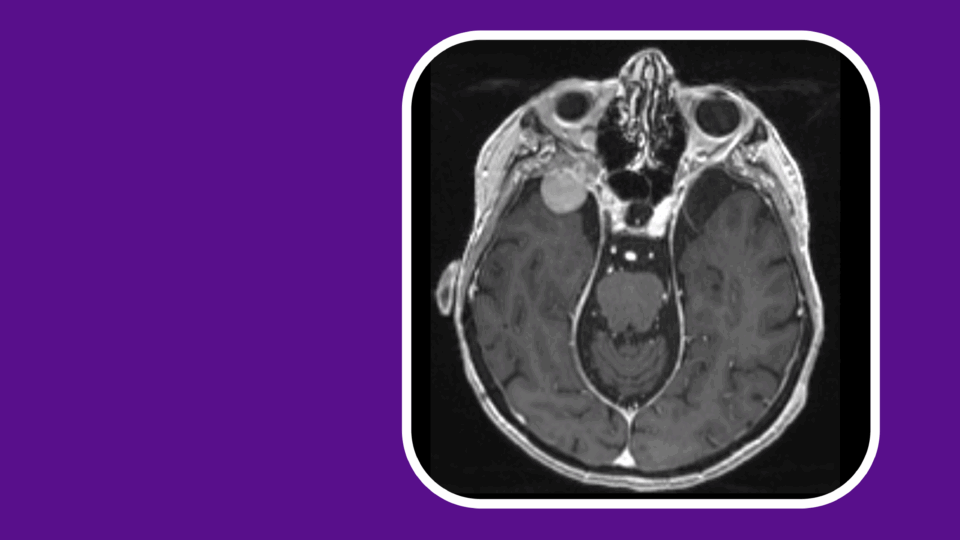
With no evidence of eye socket metastasis, the patient will continue to see Dr. Chung every six months to be monitored for eyelid recurrence.
Overall, the case can serve as an important reminder to include sebaceous carcinoma of the eyelid in the differential diagnosis, especially in older patients with an eyelid lesion or chronic inflammatory changes, Dr. Chung says.
“Beware of the great masquerader of sebaceous carcinoma of the eyelid. It can look exactly like blepharitis or chalazion,” she says.
“Have a low threshold for biopsy or referral to an oculoplastics surgeon if there are eyelid changes refractory to medical management for several months, or if there is loss of normal eyelid architecture, such as lash loss.”