Referral Notes:
- An international study suggests that an AI model applied to digital cholangioscopy may improve the accuracy, sensitivity, and specificity of diagnosing and characterizing malignant biliary strictures.
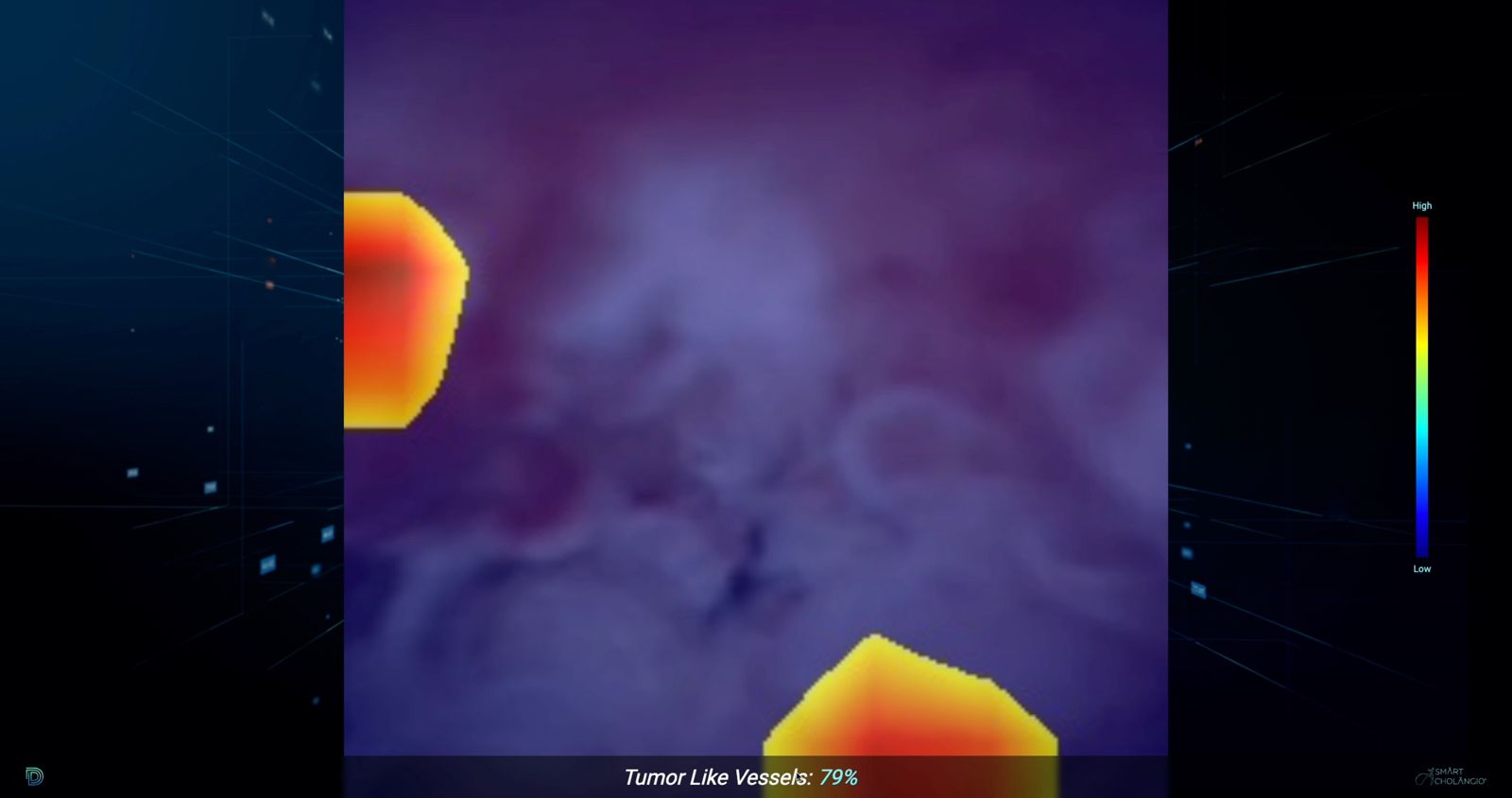
- The model may also improve biopsy targeting by generating heatmaps of malignancy-associated characteristics like papillary projections and tumor vessels.
- NYU Langone Health is the first site in the U.S. to use the model for biliary strictures and is helping adapt it to detect cancers in the pancreas and lymph nodes of the GI tract.
Differentiating between a benign and malignant biliary stricture with a cholangiogram during endoscopic retrograde chiolangiopancreatography (ERCP) can yield indeterminate results. Further characterization often requires advancing a tiny camera and forceps through the bile duct via a digital cholangioscopy, though even experienced operators can sometimes struggle to interpret the images or obtain enough tissue in the right location for a confirmative diagnosis.
“Sometimes diagnosis of a malignancy can be delayed, which is frustrating and can lead to the need for additional procedures for a patient,” says NYU Langone Health gastroenterologist Jessica Widmer, DO.
“We want to enhance tissue acquisition and make the procedure more efficient for both the patient and the physician.”
Jessica Widmer, DO
In a multicenter study in Scientific Reports, Dr. Widmer collaborated with colleagues in Portugal, Brazil, and Spain to show that an AI model applied to cholangioscopy can improve the detection and characterization of malignant biliary strictures.
“The preliminary results are quite promising,” Dr. Widmer says. “It is especially helpful in the true indeterminate biliary strictures, where it’s challenging to determine benign versus malignant changes or when the endoscopist has a strong impression, but the biopsy results do not support that impression.”
Promising Gains in Sensitivity and Specificity
Indeterminate strictures are most common in patients with primary sclerosing cholangitis (PSC), an autoimmune inflammatory condition that can eventually develop into a malignant cholangiocarcinoma, underscoring the need for better biopsies. Inflammatory masses and friability, for example, can be seen in a benign PSC, but could also be cancerous tissue.
Over the years, Dr. Widmer says, some adjunct modalities to cholangioscopy have increased the diagnostic sensitivity but compromised the specificity. By contrast, the new study found that the AI model trained on benign and malignant disease had high sensitivity and specificity.
For the study, the researchers trained and validated a convolutional neural network (CNN) on more than 96,000 images from 164 cases seen across three medical centers, and assessed its performance in detecting tumor vessels, papillary projections, nodules, and masses. Their study found that the CNN model achieved 92.9 percent accuracy, 91.7 percent sensitivity, 94.4 percent specificity, 95.1 percent positive predictive value, 93.1 percent negative predictive value, and an area under the ROC curve (AUROC) score of 0.95.
A Heatmap for Biopsies
To provide its real-time assessment of biliary tissue, the AI model interfaces with the cholangioscopy console processor via a computer app. Dr. Widmer explains that training and validating the model is an iterative process. “Videos and images captured during the procedures are used to train the model,” she says.
Beyond its overall success in detecting malignancy, Dr. Widmer notes that the model showed promise in improving tissue acquisition by identifying papillary projections with high sensitivity and specificity. “These papillary projections and tumor vessels are the most specific indicators that we have when looking for cancer,” she explains.
“It’s very promising as compared to any of the other adjunct modalities that have come down the line in the last 10 to 15 years.”
The model, in turn, provides a visual indicator of which tissue characteristics are contributing most to the algorithm’s malignancy prediction. In this heatmap, akin to a topographical map, the color red identifies the characteristics most associated with a malignancy and thus the best place to collect a biliary biopsy.
Expanding Applications
Dr. Widmer, the first provider in the United States to use the AI model to help guide biliary stricture biopsies, has begun training the model on the pancreas as well. Her team is training the model to accurately differentiate between malignant and benign cystic lesions and between solid malignancies such as neuroendocrine tumors and adenocarcinomas.
Similarly, the team is starting to train the model on benign versus malignant lymph nodes in the GI tract.
The ultimate goal, Dr. Widmer says, is to get a diagnosis as soon as possible so that patients can get appropriate therapy, while minimizing the number of procedures that they need to undergo to establish that diagnosis.
“We want to enhance tissue acquisition and make the procedure more efficient for both the patient and the physician,” she says. “This model is helping us do that, and it’s very promising as compared to any of the other adjunct modalities that have come down the line in the last 10 to 15 years.”