In July 2017, a 75-year-old cellist was struck with severe chest pain while carrying her instrument down a New York City street. After briefly losing consciousness, she was rushed to an emergency department (ED), where echocardiography revealed a grossly dilated and poorly contracting left ventricle (LV), resembling that seen in Takotsubo cardiomyopathy.
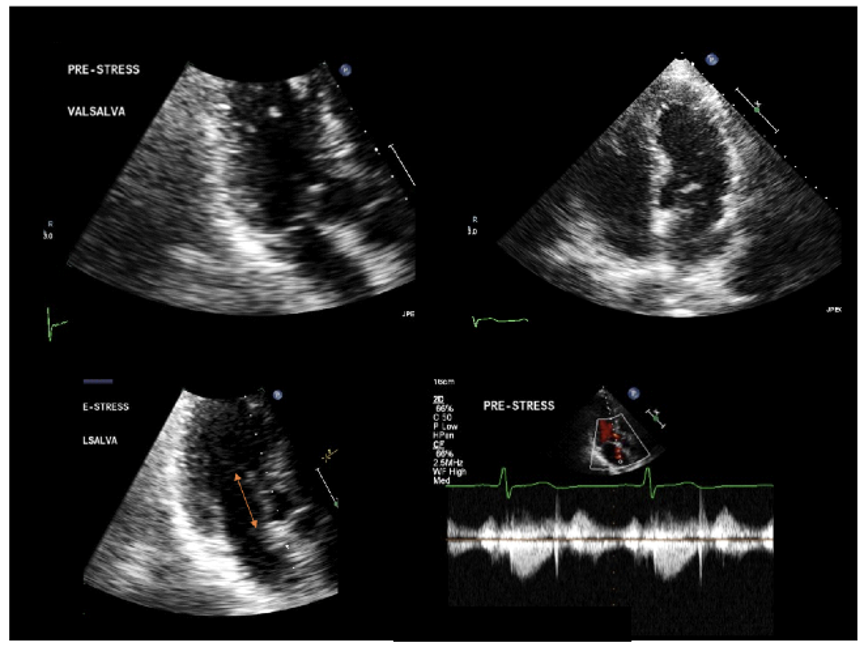
However, the ED physicians suspected that she instead had a rare, Takotsubo-like complication of obstructive hypertrophic cardiomyopathy (HCM), first reported by researchers now at NYU Langone Health—cardiogenic shock with LV ballooning secondary to outflow tract obstruction.
The woman was immediately transferred to NYU Langone, whose HCM program is among the largest in the world. There, Mark V. Sherrid, MD, the program’s director, confirmed the diagnosis. Intravenous beta blockers, vasopressin, and norepinephrine quickly resolved the acute obstruction, and the ballooning along with it.
Like many patients who experience this pseudo-Takotsubo syndrome, the cellist had not been previously diagnosed with a cardiac disorder, despite frequent shortness of breath during exertion. She was discharged on a regimen of disopyramide, whose utility in reducing left ventricular outflow tract (LVOT) obstruction was established by Dr. Sherrid and colleagues in the early 2000s. Although the medication initially controlled the symptoms she’d experienced prior to the crisis, its efficacy waned over the next five years, and she had increasing difficulty tolerating side effects.
“For the subset of patients with HCM and leaflet elongation but minimal septal hypertrophy, myectomy is often not adequate for complete relief. Our procedure offers added insurance.”
Daniel G. Swistel, MD
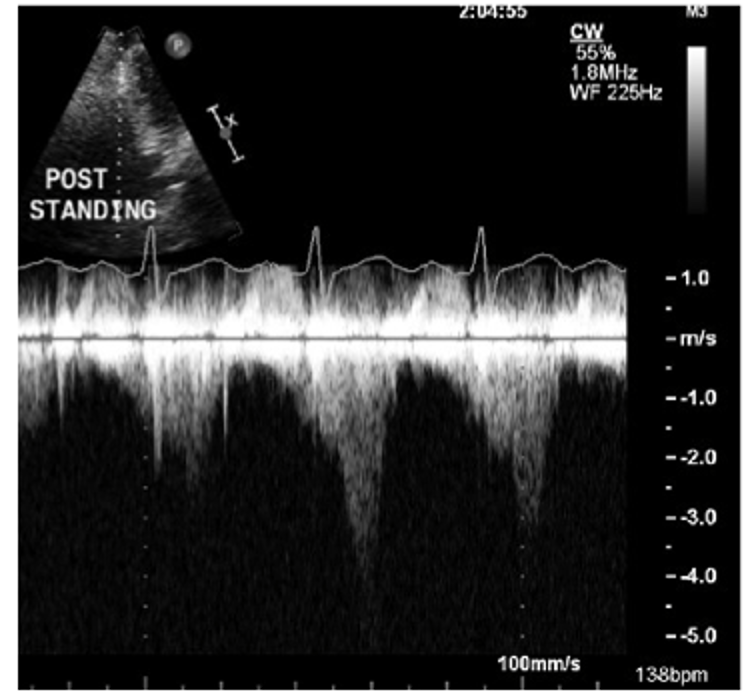
Follow-up testing with standard and stress echocardiography showed no significant outflow tract gradient. But when Dr. Sherrid ordered a postprandial stress echocardiogram, a diagnostic tool he helped pioneer, it elicited a strikingly high gradient. This suggested that the symptoms and most of the obstruction was secondary to an elongated mitral valve, rather than septal thickening. In such cases, the obstruction is more difficult to detect—and medical management often fails.
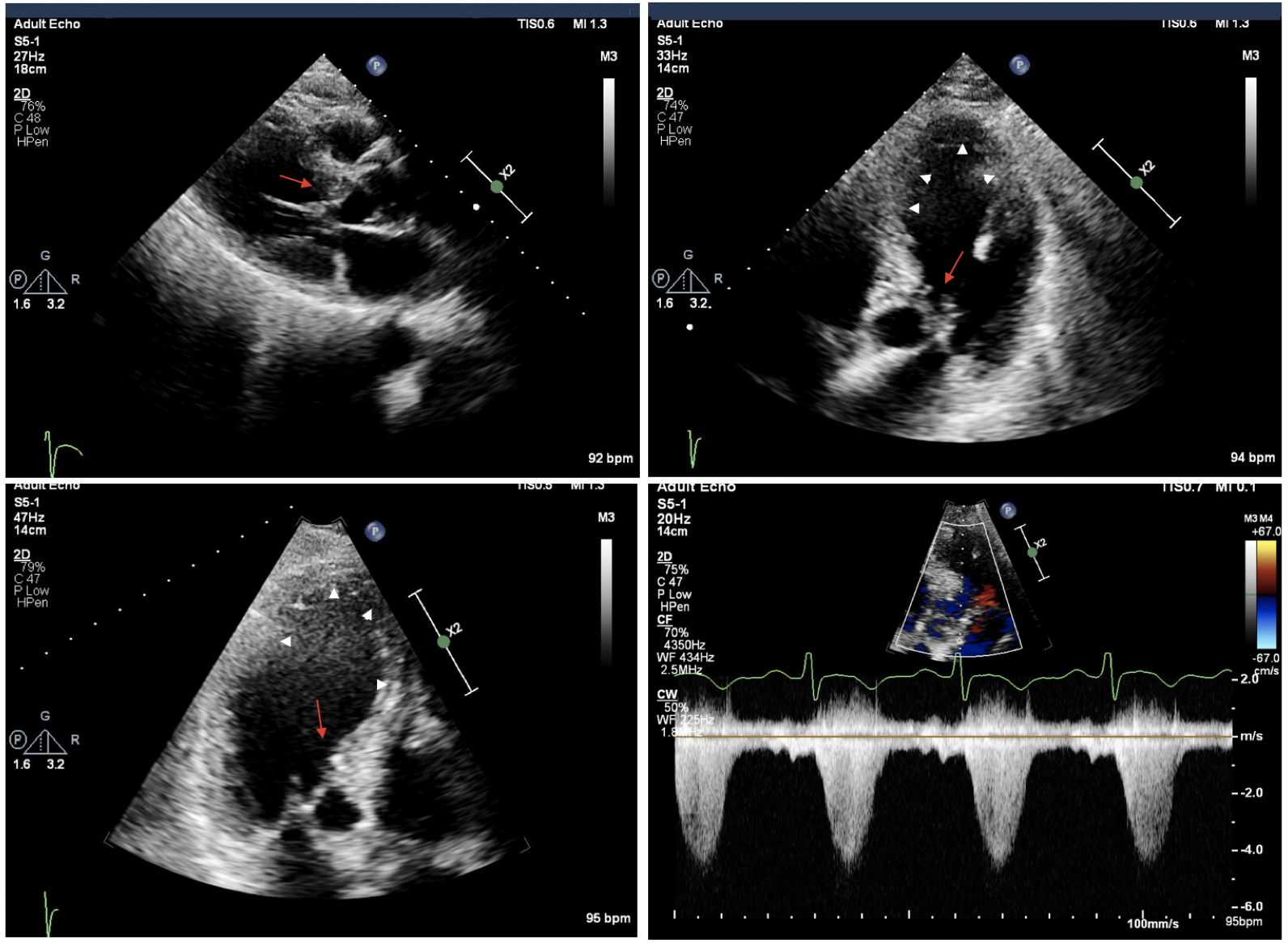
More detailed imaging revealed that the cellist’s coronary anatomy fit this pattern. “Her anterior basal septum was only slightly thickened, but her mitral valve was very long, with markedly abnormal attachments,” says Daniel G. Swistel, MD, surgical director of the HCM program. That left surgery as the only effective option to relieve her obstruction and her symptoms.
ReLex Offers Backup Benefits
For patients with HCM resistant to pharmacotherapy, surgical myectomy has long been the gold standard therapy. But the NYU Langone team judged that this patient was also a candidate for an ancillary procedure to shorten the mitral valve. Beginning in the late 1990s, Dr. Swistel pioneered the technique of horizontal anterior leaflet plication, now widely used for that purpose.
Over the past decade, he has shifted to an approach he calls residual leaflet resection (ReLex), which is suitable for patients with fibrotic or anomalous chords who are not good candidates for plication. In this procedure, the residual leaflet that protrudes past the coaptation plane is identified preoperatively on transthoracic and transesophageal echocardiography and confirmed by direct inspection. After ensuring that there is adequate chordal support to the leaflet margins on either side, the residual leaflet is carefully excised.
In a study of 416 patients with HCM recently published in the Annals of Cardiothoracic Surgery, Dr. Swistel and Dr. Sherrid and their coauthors found no significant differences in survival, gradient reduction, or mitral regurgitation after myectomy combined with ReLex or horizontal plication, or myectomy alone.
“For the subset of patients with HCM and leaflet elongation but minimal septal hypertrophy, myectomy is often not adequate for complete relief,” Dr. Swistel explains. “Our procedure offers added insurance against negative outcomes for these individuals.”
Procedure Overview
After discussions with her care team, the cellist consented to this approach. The surgery was performed in January 2022 by Dr. Swistel alongside Joshua A Scheinerman, MD, associate surgical director of the program, with Dr. Sherrid and Daniele Massera, MD, observing and offering supportive advice.
“At 83, she’s performing concerts around the world, and she carries her cello without difficulty.”
Mark V. Sherrid, MD
The patient underwent sternotomy and was placed on heart–lung bypass. Her septal thickness was measured using on-pump interoperative echocardiography (OPIE). In this technique, developed by the HCM team, a probe is inserted through the aortic valve while the right ventricle is briefly backfilled with blood to create an interface between the blood and myocardium.
After thinning the septum by less than 5 mm, the surgeons turned to the mitral valve. They resected a residual leaflet protruding more than 1 cm past the cooptation point and performed complex realignment of subvalvular attachments. Finally, the heart was closed and restarted, and the patient was transferred to the cardiac intensive care unit to begin her recovery.
The musician was discharged five days later, resumed normal activities within six weeks, and today remains symptom-free. “At 83, she’s performing concerts around the world, and she carries her cello without difficulty,” Dr. Sherrid reports. “She’s one of our most grateful patients.”
- View the Slideshow detailing a similar case where latent LVOT obstruction progressed to severe LV ballooning.
- Read the team’s study of anatomic abnormalities characteristic of hypertrophic cardiomyopathy in Takotsubo syndrome.