Referral Notes:
- Older adults with IBD have nearly double the risk of a major postoperative event as compared to younger adults.
- NYU Langone researchers are developing specific preoperative risk stratification tools for older adults undergoing intestinal resection for IBD.
- Sarcopenia, as measured by the Skeletal Muscle Index (SMI), could be a better predictor of 30-day postoperative outcomes than chronological age alone.
- If SMI proves to enhance preoperative risk stratification, early surgical intervention could be prioritized for lower-risk patients, while “prehabilitation” recommended to those at higher operative risk.
Older patients with inflammatory bowel disease (IBD) are more likely to experience adverse postoperative outcomes following IBD-related surgery as compared to younger patients. Additionally, they are more susceptible to sarcopenia, as chronic inflammation leads to accelerated muscle loss.
In a recent study published in Inflammatory Bowel Diseases, researchers led by gastroenterologist Adam Faye, MD, director of clinical research at NYU Langone Health’s Inflammatory Bowel Disease Center, explored whether assessing muscle mass could help risk stratify older adults undergoing IBD-related surgery.
“We’re shifting to a biologically-based approach, utilizing frailty and sarcopenia measures as operative risk stratification tools.”
Adam Faye, MD
“Traditionally, decisions around surgical candidacy have been made based on chronological age alone,” Dr. Faye says. “We’re shifting to a biologically-based approach, utilizing frailty and sarcopenia measures as operative risk stratification tools.”
Sarcopenia and Surgical Outcomes
Within the NYU Langone system, the researchers conducted a retrospective analysis that included 120 patients aged 60 years and older who had biopsy-proven IBD and underwent IBD-related intestinal resection between 2012 and 2022. In the cohort, they identified which measure of muscle mass had the highest predictive value for an adverse 30-day postoperative outcome and evaluated whether muscle mass was significantly associated with adverse outcomes.
“The limited research evaluating muscle mass in adult patients with IBD has yielded mixed results, partly due to the heterogeneity among measures,” Dr. Faye explains. “Cutoff values for assessments have been largely derived from non-IBD older adult populations, limiting their clinical utility.”
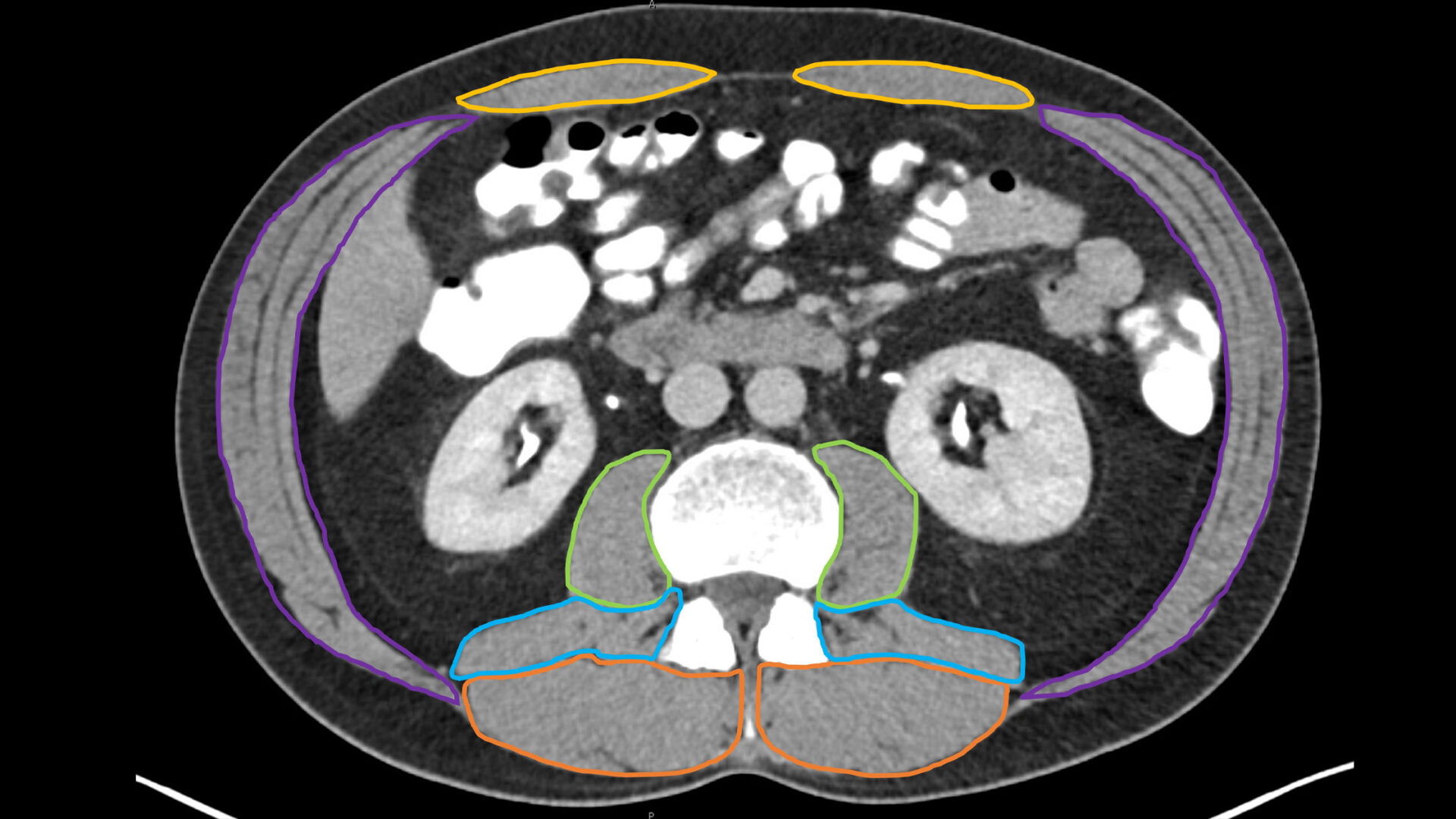
For the present study, sarcopenia was measured from preoperative imaging collected within 60 days of surgery using the Skeletal Muscle Index (SMI) and Total Psoas Index (TPI). Prior to this analysis, these indices had not been applied to older adult IBD populations.
Skeletal Muscle Mass as a Predictor
When assessing the predictive performance of SMI as compared to TPI for an adverse 30-day postoperative event, SMI had a significantly higher area under the curve than TPI (0.66 vs. 0.58).
On multivariable analysis, prior IBD-related surgery, lower skeletal muscle mass, male sex, and preoperative sepsis were all associated with a higher risk of an adverse postoperative outcome.
“The SMI may aid in preoperative risk stratification for older adults with IBD.”
“The total amount of skeletal muscle mass, as measured by SMI, was as an accurate predictor of outcomes 30 days after surgery,” says Dr. Faye. “SMI may therefore aid in preoperative risk stratification for older adults with IBD.”
A Modifiable Risk Factor
According to Dr. Faye, these findings can help shift the current paradigm of deferring surgical intervention based on chronological age alone and, as a result, reduce surgical delays among older adults at lower preoperative risk.
He explains that sarcopenia could also serve as a modifiable preoperative factor for older adults who are at higher risk for surgery, noting that “prehabilitation” protocols—incorporating exercise and nutritional support interventions—could be used to modify surgical risk to achieve better outcomes.
“Factors, such as muscle strength and nutrition, could be optimized to ready patients for IBD-related surgery.”
“Our goal is to build better risk stratification tools for surgical intervention specific to older adult IBD populations,” says Dr. Faye. “Factors, such as muscle strength and nutrition, could be optimized to ready patients for IBD-related surgery.”
In future prospective work, the researchers will continue to evaluate the added value of muscle strength and additional functional measures to aid in preoperative risk stratification of older adults with IBD.