Case Highlights:
- The patient, family, and clinical team chose embolization followed by open surgery for curative treatment of the lesion and for immediate relief of debilitating migraines.
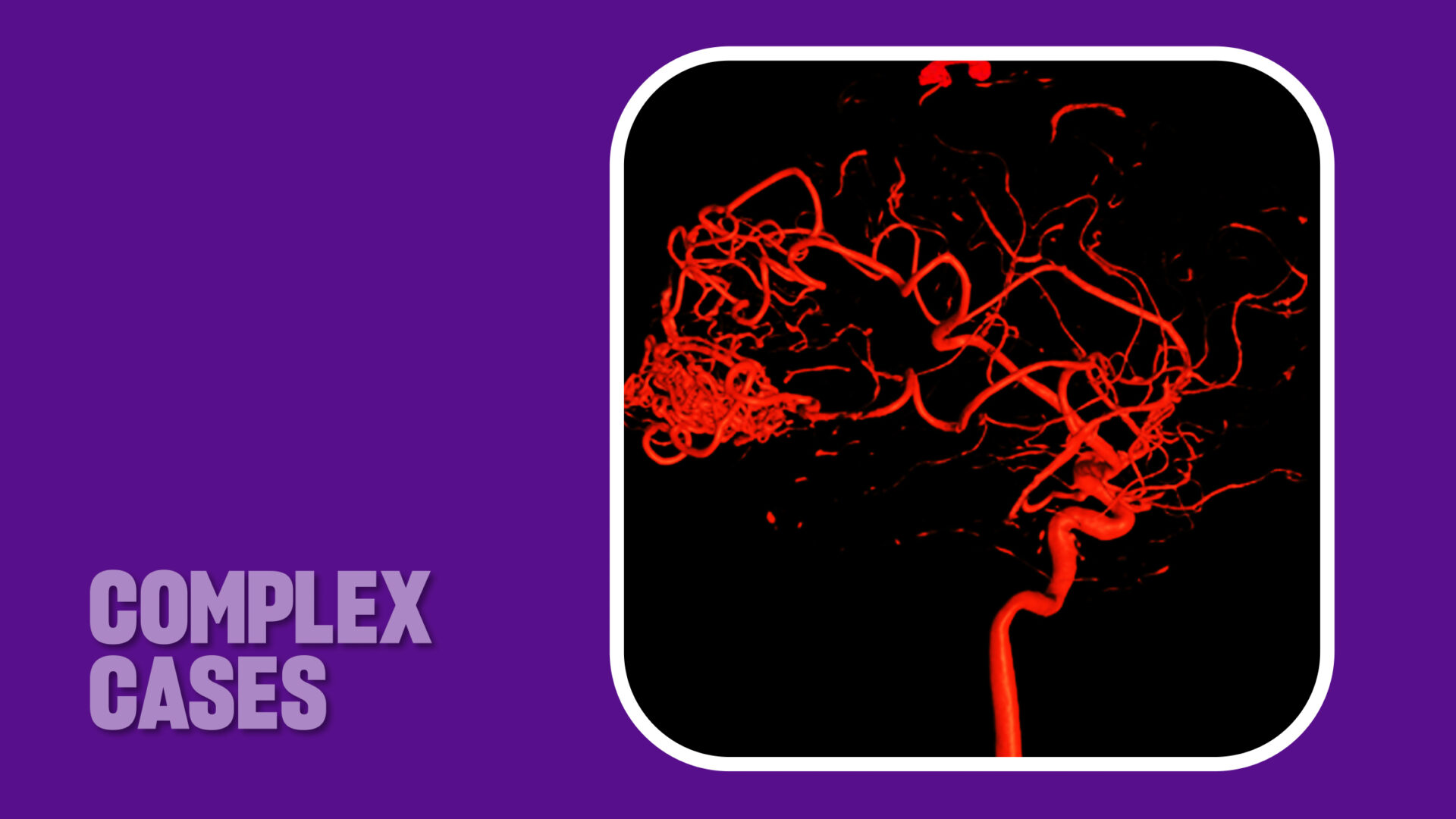
- Preoperative angiography with 3D reconstructions revealed the AVM to be 4 cm in size and at a high risk of bleeding.
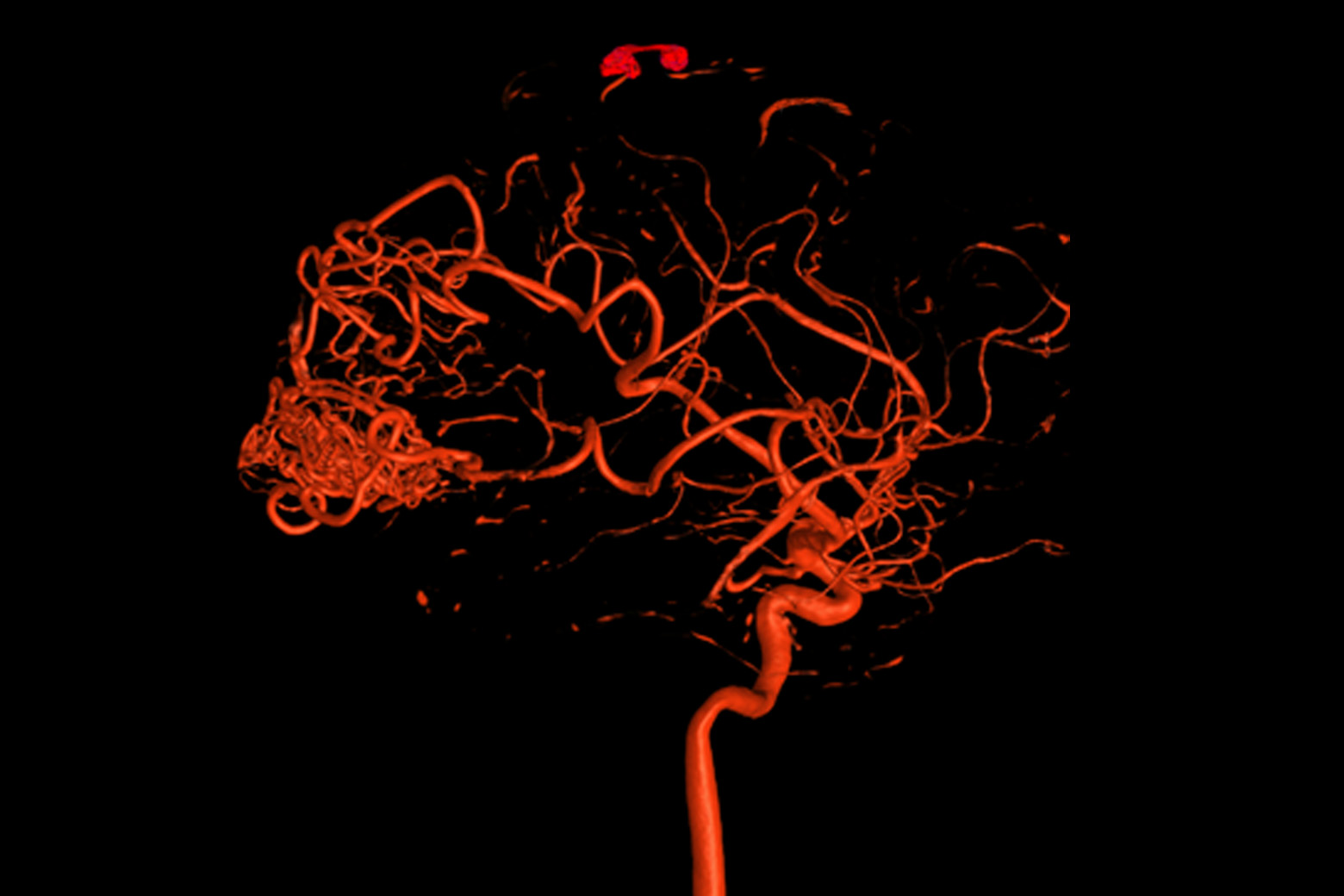
- Functional MRI with diffusion tractography mapped adjacent eloquent brain surfaces and white matter anatomy.
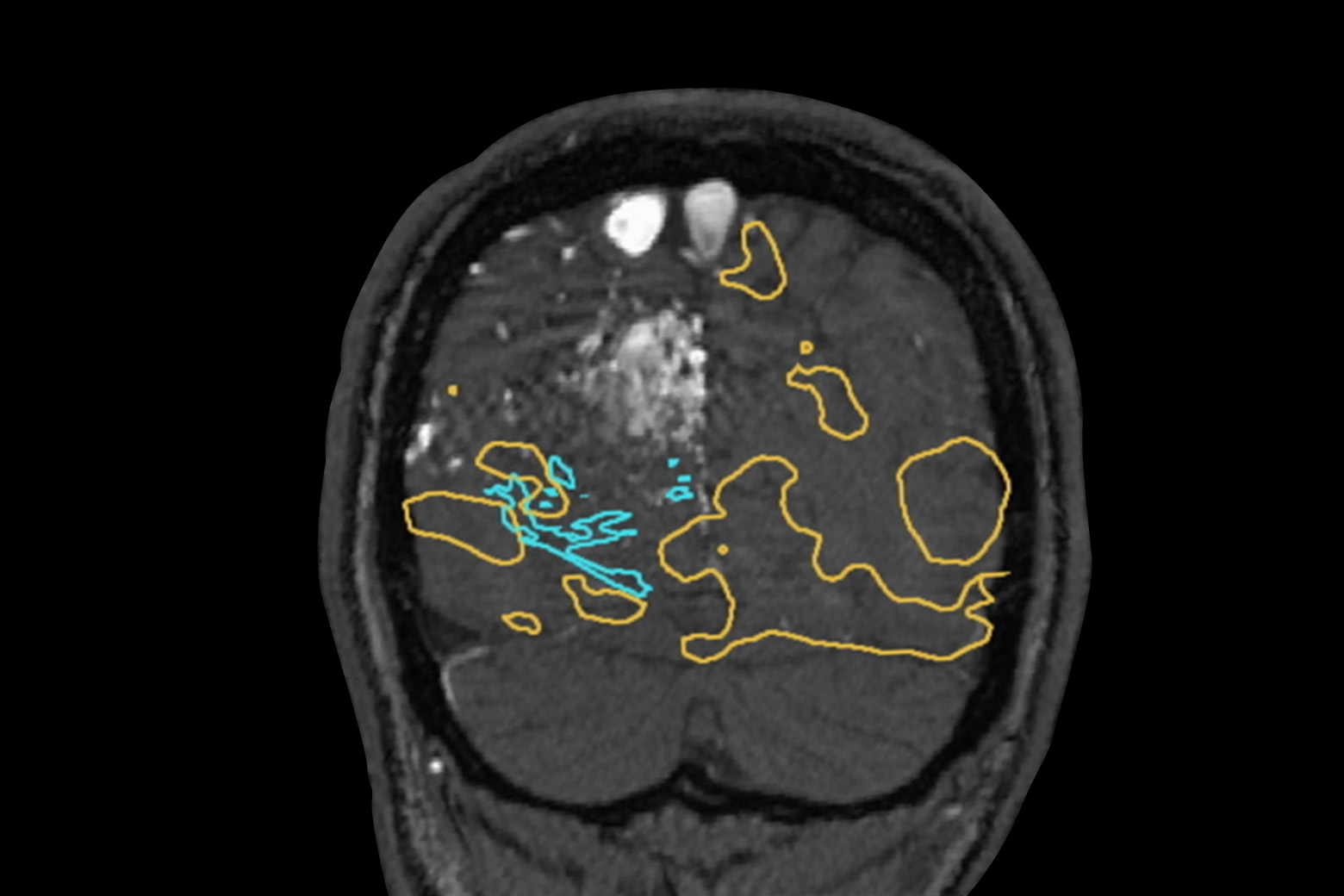
- Preoperative embolization reduced the size of the AVM nidus by about 50 percent.
After sustaining a football-related concussion in August 2023, a 15-year-old boy with a preexisting history of chronic migraines experienced worsening symptoms, severe nausea and visual defects in his left eye. His migraines increased in frequency until he was unable to attend school. Neither physical therapy nor acupuncture provided relief. And although treatment with rimegepant dulled some of his pain, it intensified his nausea.
By April 2024, an MRI revealed the cause: a large arteriovenous malformation (AVM) centered in the right occipital lobe of the patient’s brain. Following the diagnosis, the patient was referred to NYU Langone Health neurosurgeon Howard A. Riina, MD, director of the Center for Stroke and Neurovascular Diseases, for specialized care.
In just a month after Dr. Riina and his team performed open surgery to resect the lesion, the patient experienced a life-changing moment—freedom from the migraines that had plagued him for years.
Detailed Surgical Planning
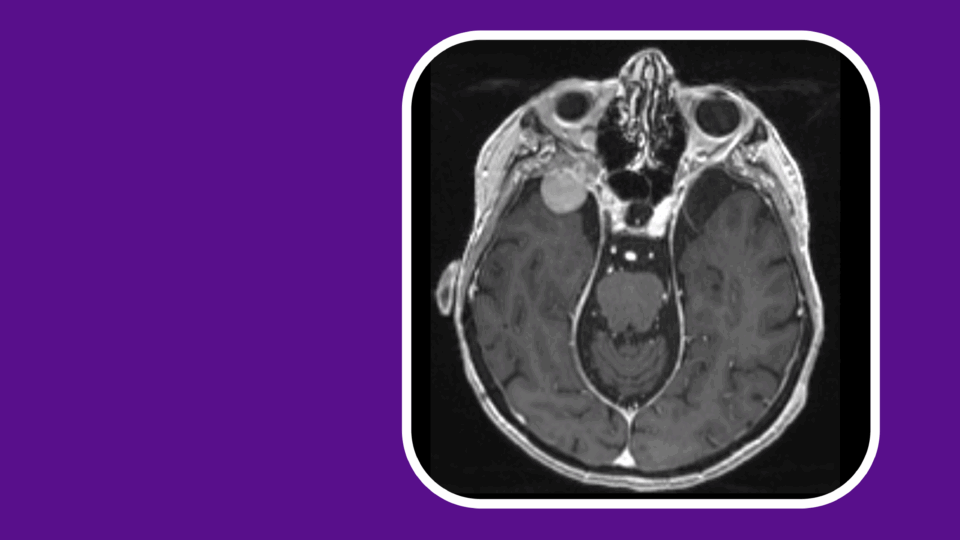
Dr. Riina initially performed diagnostic and rotational angiography with 3D reconstructions (Slide 1) to better characterize the vascular pathology and to inform clinical decision-making. The detailed imaging confirmed the exact size and location of the AVM, as well as the arterial branches feeding it. The imaging also revealed several areas of the lesion featuring a high risk for potential bleeding.
Treatment options were then presented, including surgical resection, Gamma Knife radiosurgery, and endovascular embolization, on its own or in combination with one of the other strategies. The patient and his family chose surgery combined with embolization, in part because radiosurgery sometimes requires two to four years for complete treatment response.
“We knew that resection could provide an immediate cure if the malformation was completely removed, leading to a rapid improvement of his headache syndrome.”
Howard A. Riina, MD
“Given the size and location of the AVM, his symptoms, and the significant risk of AVM-related bleeding over his lifetime, I felt that surgical resection was his best option,” Dr. Riina says. “We knew that resection could provide an immediate cure if the malformation was completely removed, leading to a rapid improvement of his headache syndrome.”
Functional MRI (fMRI) with diffusion tractography, conducted by neuroradiologist Timothy M. Shepherd, MD, PhD, confirmed that the AVM did not involve eloquent cortical regions and provided detailed mapping of the patient’s white matter anatomy (Slide 2).
“Dr. Riina and I determine eloquence based on direct fMRI visualization of patient tasks,” Dr. Shepherd says. “We also look at additional important cortical regions, like frontal eye fields and the supplementary motor area. We then map the white matter anatomy that connects all these regions.” This advanced imaging provides a more complete picture for safer treatment planning, Dr. Shepherd says.
“[We] determine eloquence based on direct fMRI visualization of patient tasks … We then map the white matter anatomy that connects all these regions.”
Timothy M. Shepherd, MD, PhD
In a preoperative embolization, Dr. Riina infused an ethylene vinyl alcohol copolymer dissolved in dimethyl sulfoxide into arterial branches feeding the patient’s AVM nidus. The procedure obliterated roughly 50 to 60 percent of the AVM nidus, as shown by an angiogram (Slide 3).
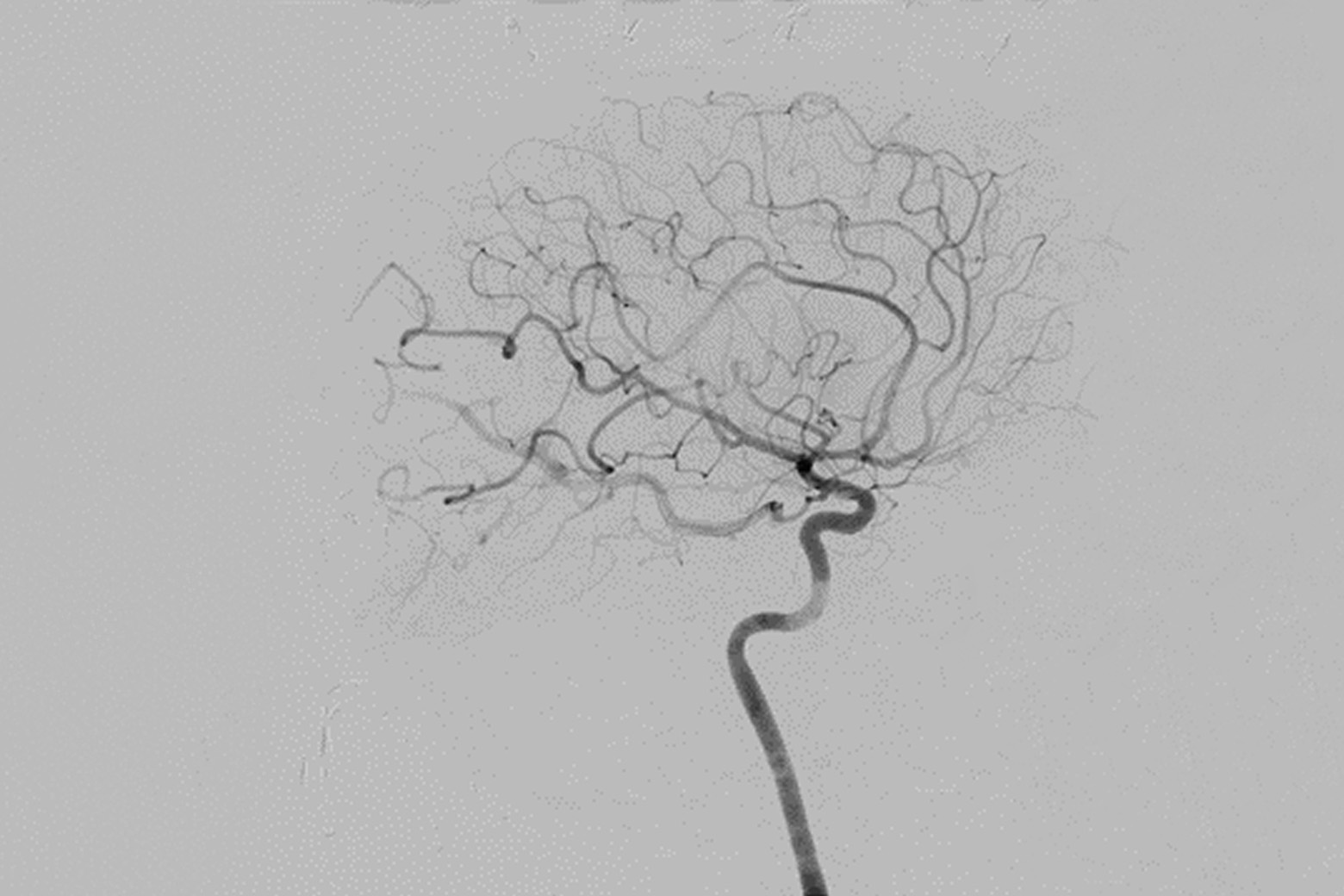
The following day, Dr. Riina performed an image-guided craniotomy and resection of the AVM. Intraoperative angiography confirmed the prior embolization and the successful resection of the remaining components of the AVM body (Slide 4). The patient’s migraines and visual field defects fully resolved after his surgery.