Bringing a breadth of expertise in interventional endoscopy, Nikhil A. Kumta, MD, recently joined NYU Langone Health as chief of endoscopy at Tisch Hospital and Kimmel Pavilion in Manhattan.
Dr. Kumta has authored more than 125 peer-reviewed articles and has helped drive innovation in minimally invasive endoscopic techniques for gastrointestinal disorders and cancers, including helping to pioneer endoscopic ultrasound-directed transgastric ERCP (EDGE) for patients with gastric bypass anatomy. He is a greatly welcomed and valued addition to the advanced endoscopy leadership team, led by Gregory B. Haber, MD, chief of endoscopy for NYU Langone Health.
Here, he discusses how third-space endoscopy and other advanced procedures are transforming patient outcomes today—and how he aims to further elevate the field in his new role.
Physician Focus: Dr. Kumta, what drew you to subspecialize in interventional endoscopy within gastroenterology?
Dr. Kumta: Following my GI fellowship, I pursued an additional year of advanced endoscopy training, where I was fortunate to work with a research team at the forefront of new endoscopic techniques. As part of this team, I was exposed to many minimally invasive, surgery-sparing endoscopic procedures. These innovative procedures, though still in their early stages, have already become a standard of care here at NYU Langone.
I was also closely involved in outcomes research associated with newer procedures and techniques, which I continued after training. The experience fueled my passion for endoscopic innovation and research—the ability to help diagnose and treat conditions in the GI tract with a less invasive procedure, faster recovery, and better outcomes.
Physician Focus: What are some of those newer procedures we offer here that are having a positive impact on patient outcomes?
Dr. Kumta: Some of the procedures becoming the standard of care here are third-space endoscopy procedures, which achieve outcomes similar to surgery but with a minimally invasive endoscopic approach. For example, peroral endoscopic myotomy (POEM) for achalasia and other motility disorders, and endoscopic submucosal dissection (ESD) for early-stage cancers of the GI tract.
“We are dedicated to expanding the availability of ESD, a procedure available at only a limited number of specialized centers across the country.”
In achalasia and other swallowing conditions, the only way to relieve the high pressure in the lower esophageal sphincter (LES) was historically to cut those muscle fibers through abdominal surgery. Now, with POEM, we can insert a scope through the mouth and advance through the esophageal wall to reach and cut those LES muscle fibers. The patient can go home the next day and have a seamless recovery with a high treatment success rate, usually in the range of 90 to 95 percent.
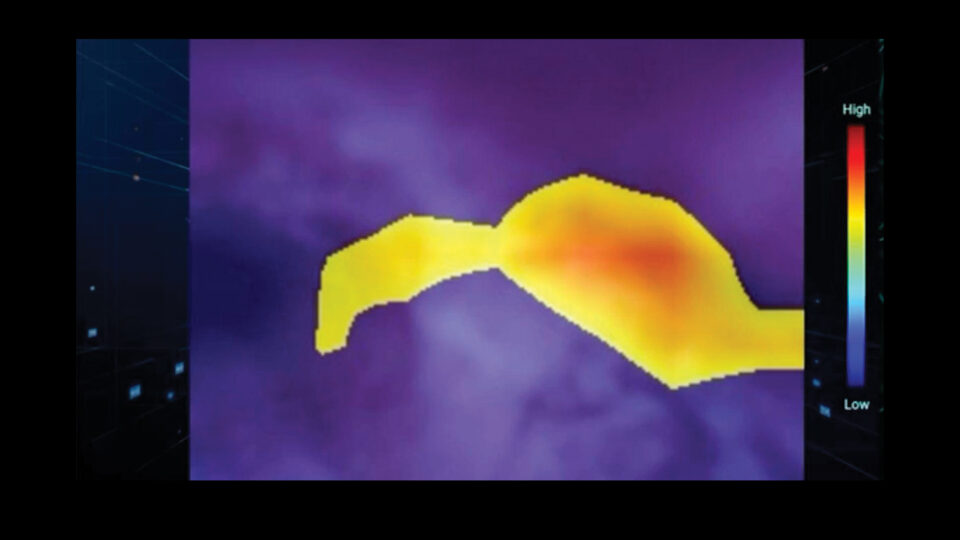
ESD is an endoscopic technique that enables en bloc resection of early-stage cancers and precancerous lesions throughout the GI tract, including the esophagus, stomach, and colon. Unlike traditional piecemeal removal techniques, ESD allows for precise excision with intact margins, significantly reducing the risk of recurrence and providing an excellent oncologic outcome. This advanced procedure often eliminates the need for surgery in select patients, offering faster recovery times and fewer complications. At NYU Langone, we are dedicated to expanding the availability of ESD, a procedure available at only a limited number of specialized centers across the country.
We also use innovative approaches to treat reflux—transoral incisionless fundoplication (TIF), for instance—and to treat obesity. These techniques are available at only a few centers in New York City or nationwide.
Physician Focus: You mentioned obesity treatment. With the availability of GLP-1 medications, are patients still pursuing traditional gastric bypass techniques for obesity?
Dr. Kumta: Absolutely, there remains a significant role for nonpharmacologic obesity treatments, including bariatric endoscopy and bariatric surgery. The GLP-1 medications have utility in treating obesity and its comorbidities, but they can be challenging to access, can come with significant side effects, and are intended for long-term, indefinite use.
Endoscopy has an important role in both primary obesity treatment, such as with endoscopic sleeve gastroplasty (ESG), and in the long-term management of patients who undergo bariatric surgery.
“Endoscopy has an important role in both primary obesity treatment, such as with ESG, and in the long-term management of patients who undergo bariatric surgery.”
For example, during my training, I was closely involved in developing a procedure known as EDGE—endoscopic ultrasound-directed transgastric ERCP. Accessing the bile duct in patients with prior gastric bypass surgery can be extremely challenging endoscopically. Due to the bypass anatomy, we can’t easily advance a scope across the stomach into the small intestine where the bile duct empties. For patients who present with issues like stones, the EDGE procedure can be used to place a dumbbell-shaped stent between the gastric pouch and the excluded stomach, providing a conduit that enables us to insert a traditional scope through the stent for treatment.
Physician Focus: Can you discuss recent trends in esophageal and gastric cancer, and how advancements in endoscopic procedures are changing patient outcomes?
Dr. Kumta: As with colon cancer, we are seeing overall rises in esophageal and gastric cancer incidence. Although the United States does not have universal esophageal and gastric cancer screening programs, at NYU Langone we treat patients from around the world, including from countries where gastric cancer incidence is higher and nationwide screening is in place. As a result, we see patients referred to us after a positive screening exam, as well as those whose early gastric cancers are found when they’ve had an endoscopy for other symptoms, such as reflux.
“Our goal is to keep opening new possibilities in the endoscopic treatment of our patients—possibilities that were once unimaginable.”
While many of these patients previously would have needed a major surgery to remove either part or all of their stomach, we’re able to offer them a minimally invasive, organ-sparing treatment like ESD to remove their early-stage cancer and provide them with an endoscopic cure. One area of my ongoing research aims to identify the types and size of tumors best suited for endoscopic resection.
Physician Focus: What are your priorities in your new appointment as chief of endoscopy?
Dr. Kumta: One of the things that drew me to NYU Langone is the opportunity to help lead a cutting-edge endoscopy program where we can continue to enhance patient outcomes and help set new standards in care. I look forward to collaborating across specialties—in gastroenterology, oncology, interventional radiology, radiation oncology, and beyond—to continuously improve outcomes for GI cancers and other conditions using endoscopic procedures. Our goal is to keep opening new possibilities in the endoscopic treatment of our patients—possibilities that were once unimaginable.