NYU Langone’s adult neurology residency program, one of the country’s largest, is expanding to meet growing demand. In the next recruitment cycle, the program anticipates accepting 13 residents to train in Manhattan, 5 in Brooklyn, and 3 on Long Island .
Here, program director Arielle M. Kurzweil, MD, discusses the distinctive program features—shaped by NYU Langone’s location and approach to patient care—that position it as a top choice for neurologists-in-training. She also details how the program’s innovative curriculum prepares trainees for telehealth, leadership, and other essential skills.
The Lure of Diverse Cases and Cutting-Edge Tech
Physician Focus: Dr. Kurzweil, NYU Langone’s adult neurology residency program attracts trainees from across the globe. What stands out about the program?
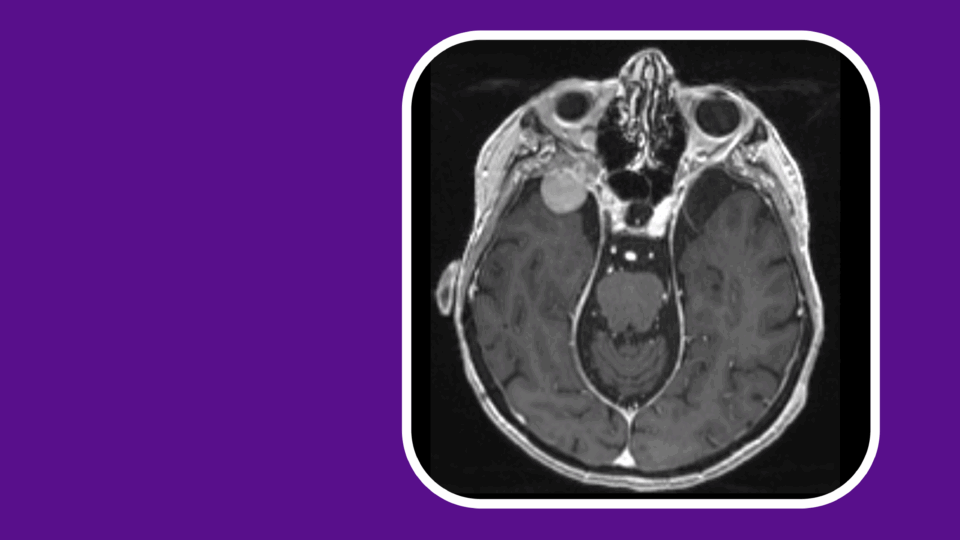
Dr. Kurzweil: One big draw is the diversity—of New York City’s population and of the unparalleled diversity of cases we see, from simple to highly complex neurological disorders. Our residents regularly encounter the kind of “unicorn” cases that a practicing neurologist might never see in their career, while also gaining exposure to our subspecialty programs, such as neurosurgical and stroke care.
Another draw is our institutional knowledge and innovative approach to care. Put simply, the same reasons patients seek care here—our high degree of expertise and access to the latest diagnostic and treatment tools—also draws neurologists-in-training.
“The same reasons patients seek care here—our high degree of expertise and access to the latest research and diagnostic and treatment tools—also draws neurologists-in-training.”
Arielle Kurzweil, MD
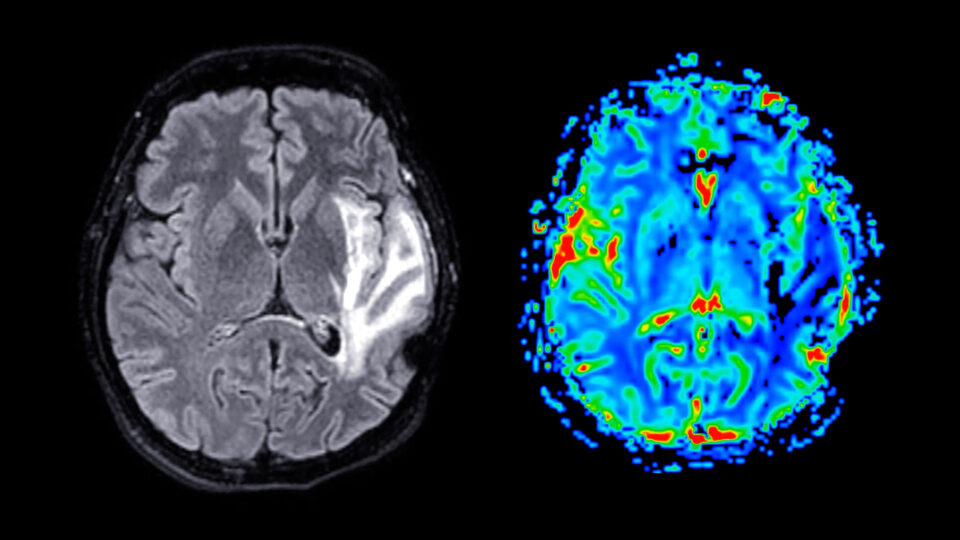
By nature of our approach, our residents develop familiarity with advanced tools such as neuromodulation and high intensity focused ultrasound for movement disorders, and transcranial direct current stimulation for multiple sclerosis. They also observe procedures that are unique to NYU Langone, such as complex epilepsy surgeries through our Comprehensive Epilepsy Center —one of the country’s largest centers for focused epilepsy care.
Exploring Unique Interests
Physician Focus: The program also offers electives and specific ‘tracks’ to residents interested in focusing their training. Can you tell us about those?
Dr. Kurzweil: For residents with a particular interest in global health or who just want to understand the specialty in a global context, we offer specialty training through the Division of Global Health. Two residents per year accompany division director Jaydeep M. Bhatt, MD, to resource-constrained countries such as Ghana and Uganda. Since neurology is a rare specialty in those areas, the residents gain the experience of both providing patient care with limited resources and educating fellow clinicians to do the same.
Additionally, we offer both an education and a research track, with one resident per class in each track. In the education track, a resident interested in a career that incorporates medical education can further develop their teaching skills and work on an education-related project with a mentor. In the new research track, a resident takes on research more expansively, with dedicated time and mentoring to develop a project and scholarly publication.
All of our trainees gain exposure to applied research through our patient-oriented research curriculum. That curriculum is integrated into our training throughout the year, providing residents with an overview of the basic principles of neurology research—and how they apply to clinical care.
Practicing the Science—and Art—of Patient Care
Physician Focus: Neurologic disease can present with a wide range of symptoms, and many rare diseases fall within the specialty as well. How do you prepare residents to pinpoint a diagnosis and then manage often-complex cases?
Dr. Kurzweil: The multidisciplinary nature of NYU Langone yields the type of collaboration that is often needed to reach a diagnosis, particularly in rare or unsolved cases, and we come together quarterly to discuss those cases. We also emphasize to our residents that they need more than procedural skills in neurology to manage challenging cases and situations, they also need communication and interpersonal skills.
“We also emphasize to our residents that they need more than procedural skills in neurology to manage challenging cases and situations, they also need communication and interpersonal skills.”
Our New York Simulation Center for the Health Sciences (NYSIM) is a valuable resource that helps our residents develop these communication skills, ensuring they are well prepared for both the science and art of neurology practice. In addition to learning to run stroke codes or perform lumbar punctures in the center, they get to practice patient encounters and interactions with nurses and emergency department doctors.
For example, residents interact with an actor playing the role of a patient whose workup indicates amyotrophic lateral sclerosis. In a live simulation, a resident experiences what it’s like to deliver that difficult diagnosis and discuss next steps, refining their delivery as needed to ensure sensitivity and compassion along with medical accuracy.
The need for these complementary skills has also grown with the increased use of telemedicine, particularly since the pandemic. Our teleneurology training guides residents through the nuances of a virtual exam, which they also practice through simulation center sessions.
Fostering a Supportive Environment
Physician Focus: What about the residents themselves—what initiatives help to make the experience of training at NYU Langone resident-centric?
Dr. Kurzweil: It’s important to us that residents to feel supported and engaged throughout their training here.
Our chief resident leadership curriculum supports residents transitioning to chief resident roles. These residents work alongside program leadership to manage various aspects of the program, and they serve as role models for junior trainees. The one-day curriculum for rising chief residents includes discussion of key leadership topics, followed by a simulation activity in which residents navigate challenging hypothetical situations with junior trainees and faculty. We were asked to present on this unique program at the American Academy of Neurology’s annual meeting earlier this year.
We also take a deliberate approach to mentorship, fostering connections between faculty and residents, as well as between senior and junior residents. It’s part of our proactive approach to enhance the residency experience and prevent burnout. We even have a simulation on this topic, in which residents are challenged to identify signs of burnout in colleagues.
Physician Focus: What is one of the most important lessons you’ve learned as program director?
Dr. Kurzweil: Overall, in my eight years as program director, I have learned that running a training program is a real team effort. Recruiting team-oriented trainees—and cultivating that team spirit—is crucial to success.
Importantly, we work to balance inpatient and outpatient neurology training and optimize trainee education, emphasizing flexibility and openness to feedback and change. As a result, residents who graduate from our program tend to embody that sense of openness and adaptability as they move forward into their careers.