Histotripsy represents a potential paradigm shift in the management of small renal masses, offering a completely noninvasive, nonthermal, and nonsurgical treatment option that addresses many of the limitations of current ablative techniques.1
The #HOPE4KIDNEY trial is the pivotal clinical trial of histotripsy for renal tumors, building upon the success of the #HOPE4LIVER trials that led to FDA approval for hepatic applications. As of June 2025, enrollment was complete with 67 subjects across 16 U.S. centers. Results are expected to support an upcoming regulatory submission to expand histotripsy use to treat kidney tumors.
Our department has unique experience with histotripsy for small renal masses and, as long-standing leaders in kidney cancer management, served as the highest enrolling site in the trial (17 patients).
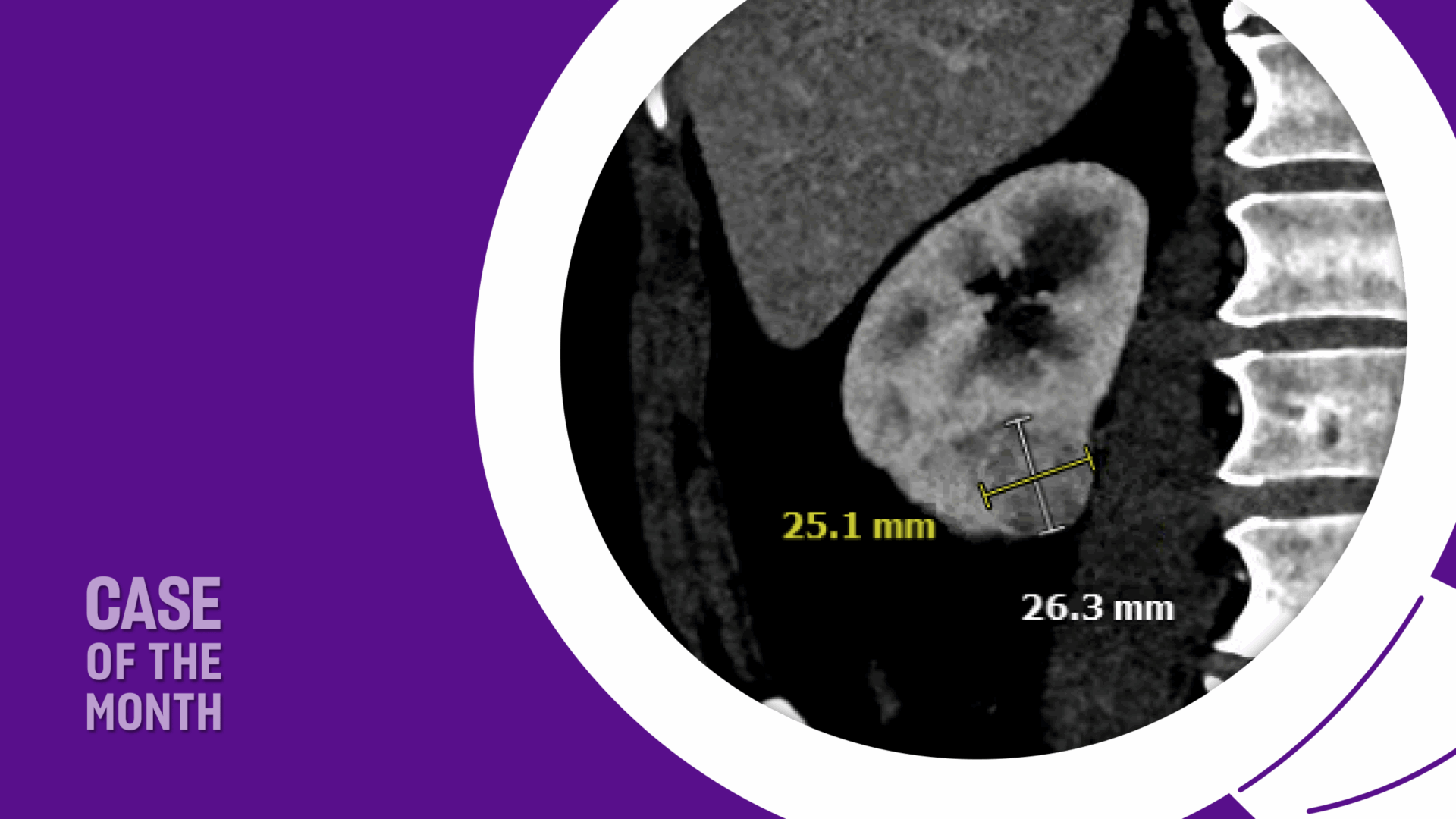
In this Case of the Month, we highlight the successful use of histotripsy to treat a 2.7-cm right renal mass. The noninvasive approach provided a valuable option for the 74-year-old patient with multiple comorbidities, including prior cerebrovascular accident, coronary artery disease with prior myocardial infarction, chronic obstructive pulmonary disease, and diabetes mellitus.
Case Highlights:
- The patient was initially monitored with active surveillance, but after imaging revealed tumor growth from 2.1 to 2.7 cm, he elected histotripsy treatment and enrolled in #HOPE4KIDNEY.
- Histotripsy was completed in under one hour with real-time ultrasound guidance.
- Post-treatment imaging confirmed tumor liquification, preserved collecting system, and no hemorrhage; the patient was discharged the same day.
- The Discussion section details histotripsy’s mechanical mechanism, selective parenchymal destruction with sparing of collagen-rich adjacent vital structures, and potential abscopal effects with future applications.
Patient Case
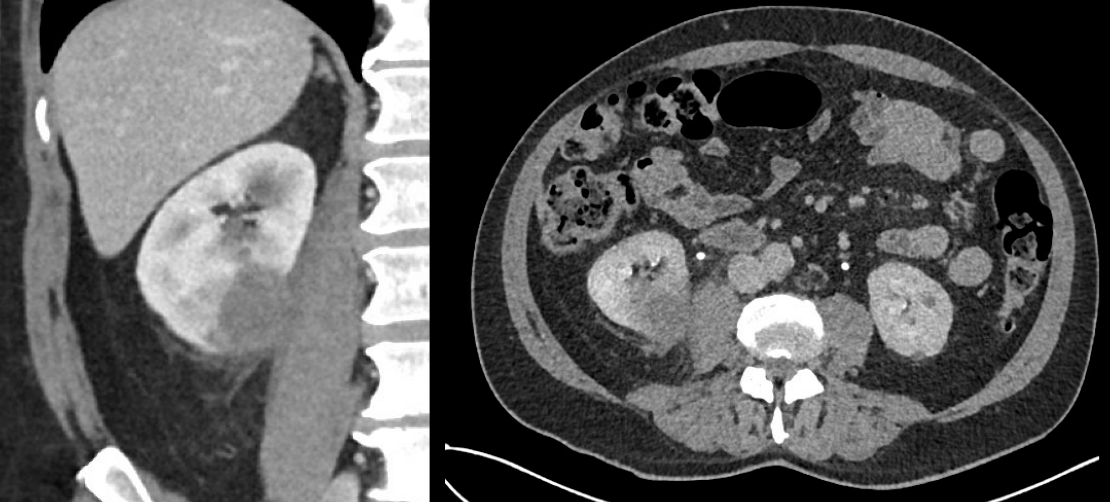
A 74-year-old male with a past medical history significant for cerebrovascular accident, coronary artery disease with prior myocardial infarction, chronic obstructive pulmonary disease, and diabetes mellitus, presented in the spring of 2024 for evaluation of an incidental 2.1-cm right renal mass discovered during work-up for microscopic hematuria. The endophytic mass was in the lower pole, up against the collecting system and demonstrated enhancement consistent with renal cell carcinoma (NS – 8). He had a serum creatinine level of 0.82 mg/dL and an eGFR of 92 mL/min/1.73m2, suggesting normal kidney function.
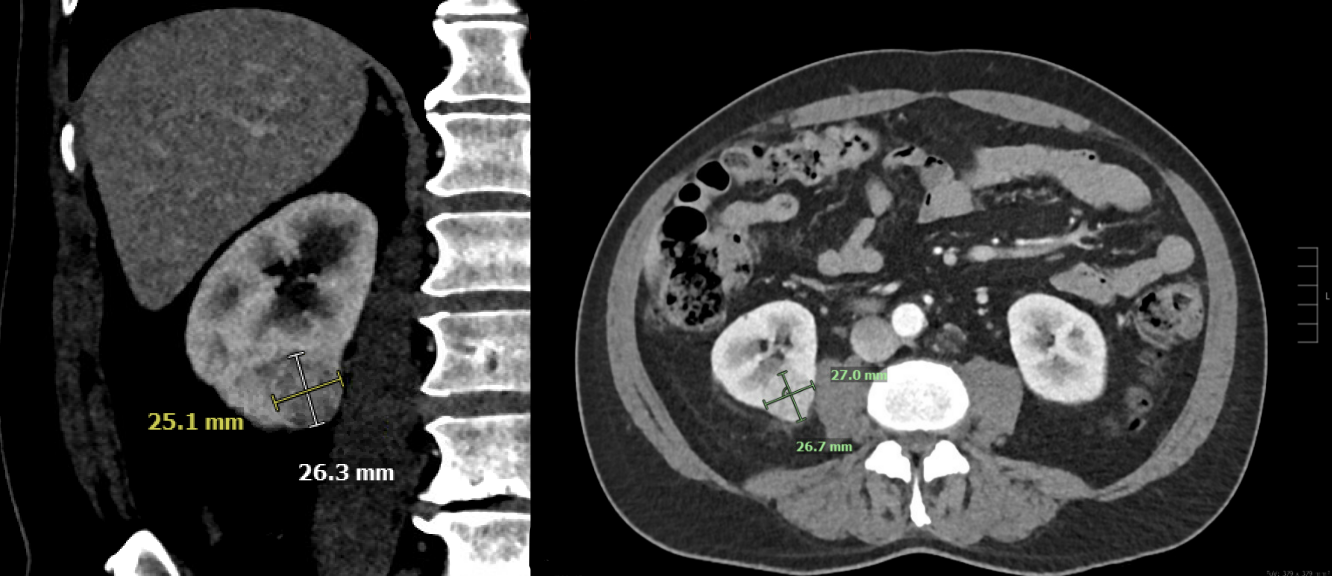
Given his significant comorbidities, he was placed on active surveillance. However, follow-up imaging over the next 12 months demonstrated continuous interval growth to 2.7 cm (Figure 1).
Management
The patient was again given the treatment options of continued observation versus percutaneous ablation versus partial nephrectomy. He was also noted to be eligible for participation in the #HOPE4KIDNEY trial evaluating histotripsy for the treatment of small kidney tumors. The eligibility criteria for the trial included a biopsy-proven, solitary, ≤ 3 cm kidney tumor not in contact with the renal hilum or renal pelvis/ureter. Other eligibility criteria included an eGFR > 45 mL/min/1.73m² and an ECOG performance score of 0 to 2.
Following an extensive treatment discussion, the patient elected to proceed with participation in the #HOPE4KIDNEY trial. Pre-procedural biopsy confirmed clear cell renal cell carcinoma, Fuhrman grade 2. The patient underwent treatment in the spring of 2025 with histotripsy using the Edison System under real-time ultrasound guidance. Unlike percutaneous ablation techniques which rely on thermal tissue destruction by passing probes or needle devices into the tumor, histotripsy is completely noninvasive and employs focused ultrasound pulses to create controlled cavitation bubbles that mechanically liquefy target tissue at the subcellular level.
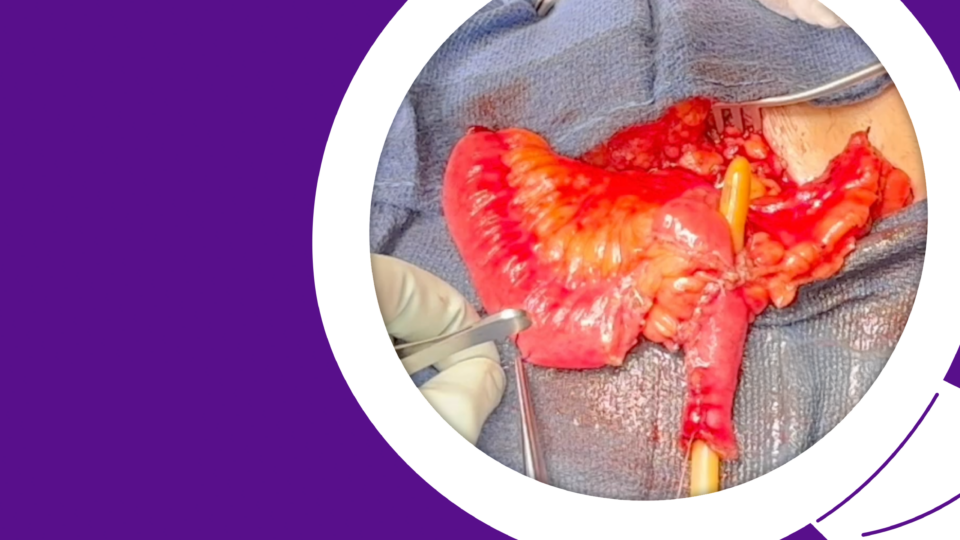
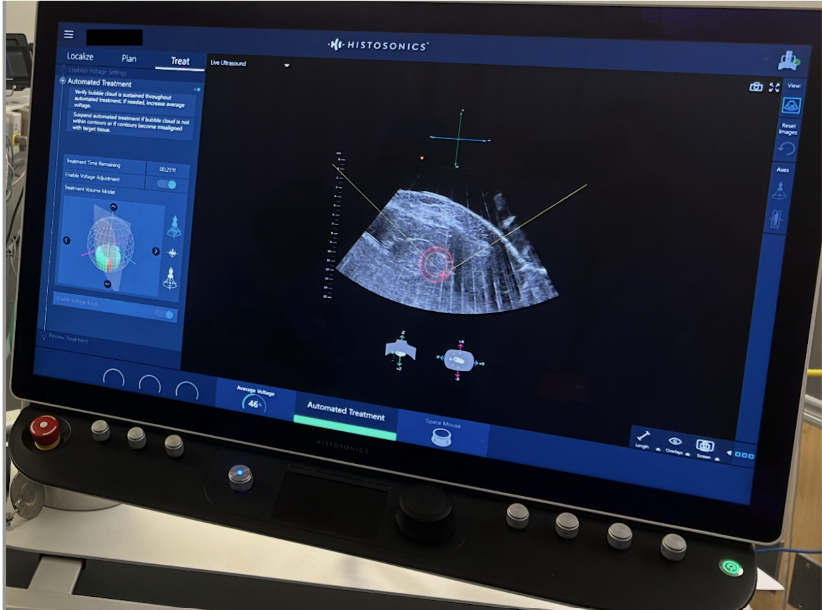
The 53-minute procedure was performed in collaboration with interventional radiologist Mikail Silk, MD, under general anesthesia with the patient positioned in lateral decubitus position. The histotripsy transducer was positioned in a water bath which is in contact with skin surface overlying the abdomen (Figure 2) and focused ultrasound pulses were delivered to mechanically fractionate the tumor tissue while preserving the surrounding collecting system and vascular structures.

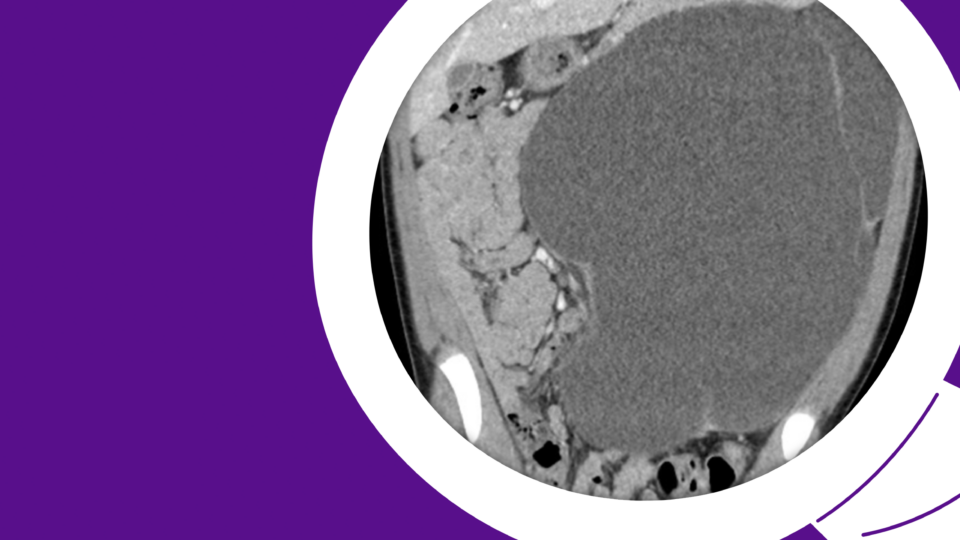
Real-time ultrasound monitoring during the procedure enabled visualization of the treatment zone (cavitation bubble cloud) and immediate assessment of treatment efficacy (Figure 3). Post-procedural imaging demonstrated complete mechanical liquefaction of the target lesion with a 5-mm margin of ablated tissue around the tumor.
The patient tolerated the procedure without difficulty and was discharged to home a few hours later without any prescription medication.
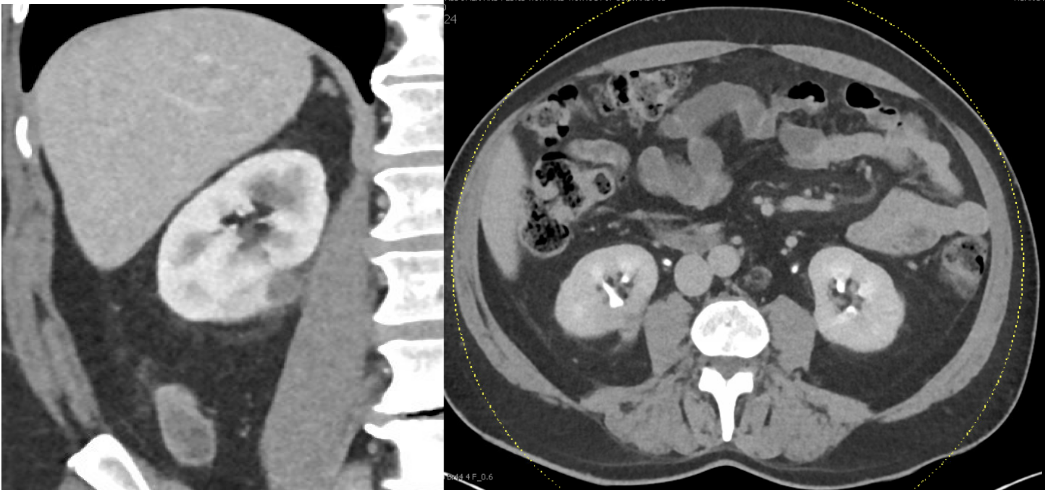
Immediate post-treatment imaging demonstrated liquefaction of the tumor with preservation of the collecting system and no evidence of significant post-treatment hemorrhage (Figure 4). Immediate post-treatment labs demonstrated a serum creatine of 0.89 mg/dL and an eGFR of 91 mL/min/1.73m².
Follow-up imaging at three months demonstrated preservation of blood vessels and collecting system with absorption of the liquefied tissue debris and no evidence of local recurrence or residual enhancing tissue (Figure 5). His renal function remained stable with an eGFR of 90 mL/min/1.73m².
Discussion
This case demonstrates the successful application of histotripsy in a clinical scenario where traditional approaches could carry additional risks of treatment-related morbidity, particularly in an unhealthy patient. The combination of noninvasive, image-guided treatment delivery, tissue selectivity, absorption of treated tissue, and potential immunological benefits positions histotripsy as a transformative technology that may redefine the management of localized and even metastatic kidney tumors.
Mechanism of Action. The fundamental advantage of histotripsy lies in its unique mechanism of action. Unlike radiofrequency ablation or cryoablation, which rely on thermal effects, histotripsy employs focused ultrasound pulses to create controlled cavitation bubbles that mechanically liquefy tissue at the subcellular level.2 This nonthermal mechanism eliminates the risk of thermal injury to adjacent structures and is not affected by heat sink effects from nearby vessels.3,4 The lack of heat makes this treatment unique to other ultrasound-based treatments such as high-intensity focused ultrasound (HIFU).
Tissue Selectivity. The tissue selectivity of histotripsy is particularly valuable for soft tissue applications such as the kidney. Collagen-rich structures such as the collecting system, blood vessels (>300 μm), nerves, and bile ducts have significantly higher mechanical resistance to histotripsy-induced damage compared to cellular parenchymal tissue.5 This differential allows for precise tumor destruction while preserving critical structures, enabling treatment of centrally located tumors that would be contraindicated for conventional thermal ablation.2
Absorption of Treated Tissue. The absorption and remodeling process following histotripsy is superior to thermal ablation techniques. The mechanically liquefied tissue debris is absorbed by the body within months, leaving minimal scar tissue (Figure 6).3 This contrasts with thermal ablation, which leaves thermally denatured tissue that can complicate surveillance imaging and may persist indefinitely.

Abscopal Effects. Histotripsy also offers unique treatment advantages beyond just noninvasive tissue destruction. The mechanical destruction of tumor cells releases intact intracellular tumor antigens and damage-associated molecular patterns (DAMPs) that can stimulate systemic immune responses.2,6 Preclinical studies have demonstrated that histotripsy can induce abscopal effects, where treatment of one tumor leads to regression of distant untreated tumors through enhanced immune activation.6 Subsequently, the future of histotripsy extends beyond local tumor control. Ongoing research includes a clinical trial investigating its potential to enhance immunotherapy efficacy through the release of intact tumor antigens and immune-stimulating agents. The combination of local tumor control with systemic immune activation may represent a new paradigm in cancer treatment, particularly for metastatic disease where conventional ablation offers limited benefit.7
Safety Profile. The safety profile of histotripsy is superior to thermal ablation techniques. Preclinical studies comparing histotripsy to cryoablation in porcine kidney models demonstrated significantly reduced bleeding complications with histotripsy (11 vs. 89 percent perirenal hematoma rate).8 The noninvasive nature of histotripsy eliminates risks associated with percutaneous approaches, including needle tract seeding, infection, and vascular injury.1 The #HOPE4LIVER trial demonstrated histotripsy’s effectiveness in disrupting liver tumors (95 percent technical success rate) with no injury to bile ducts or segmental blood vessels.9
Real-Time Monitoring. Real-time treatment monitoring is another significant advantage of histotripsy. The cavitation bubble cloud can be visualized in real-time using ultrasound imaging, allowing immediate assessment of treatment efficacy and precise control of the ablation zone.3 This capability enhances treatment precision and reduces the risk of incomplete treatment or damage to adjacent structures.
References:
- Xu Z, et al. Int J Hyperthermia. 2021;38(1):561-575. DOI.
- Xu Z, et al. Annu Rev Biomed Eng. 2024;26(1):141-167. DOI.
- Lake AM, et al. J Urol. 2008;179(3):1150-1154. DOI.
- Lundt JE, et al. Ultrasound Med Biol. 2017;43(12):2834-2847. DOI.
- Styn NR, et al. Urology. 2012;80(3):724-729. DOI.
- Hendricks-Wenger A, et al. Front Oncol. 2021;11:681629. DOI.
- Qu S, et al. J Immunother Cancer. 2020;8(1):e000200. DOI.
- Couillard AB, et al. J Vasc Interv Radiol. 2023;34(11):1986-1996. DOI.
- Mendiratta-Lala M, et al. Radiology. 2024;312(3):e233051. DOI.