On February 9, 2024, NYU Langone’s Cochlear Implant Center celebrated the 40th anniversary of its first surgical cochlear implant. Since its start, the center has been involved in testing every major cochlear innovation and has implanted roughly 5,000 devices in patients ranging from 4 months to 97 years old.
Here, center co-directors Sean O. McMenomey, MD, and William H. Shapiro, AUD, discuss the important lessons learned from their decades of experience. In addition, they describe the center’s central role in advancing other procedures like auditory brainstem implants, skull base surgery, and nonsurgical regeneration of tympanic membranes.
Decades of Change with Cochlear Implants
Physician Focus: Cochlear implants have certainly evolved since you first started implanting them in 1984. Can you reflect on these advances?
Dr. McMenomey: Our colleague Dr. J Thomas Roland Jr. has done a monumental amount of work on advances in electrode array design. I think we’ve been involved in every single advancement of electrode arrays for years. A modern cochlear implant is now beautifully thin, much thinner than the ones of yore: I used to put implants in that were at least three times thicker.
Physician Focus: How has your pool of eligible patients changed?
Dr. Shapiro: When we began implanting these cochlear devices, adult patients with bilateral hearing loss couldn’t have any hearing at all because we didn’t know what we could guarantee. The technology and selection criteria have changed dramatically since then, and we can now help a much wider spectrum of patients. The typical adult with hearing loss is a candidate for a cochlear implant if their speech discrimination is less than 60 percent with a hearing aid.
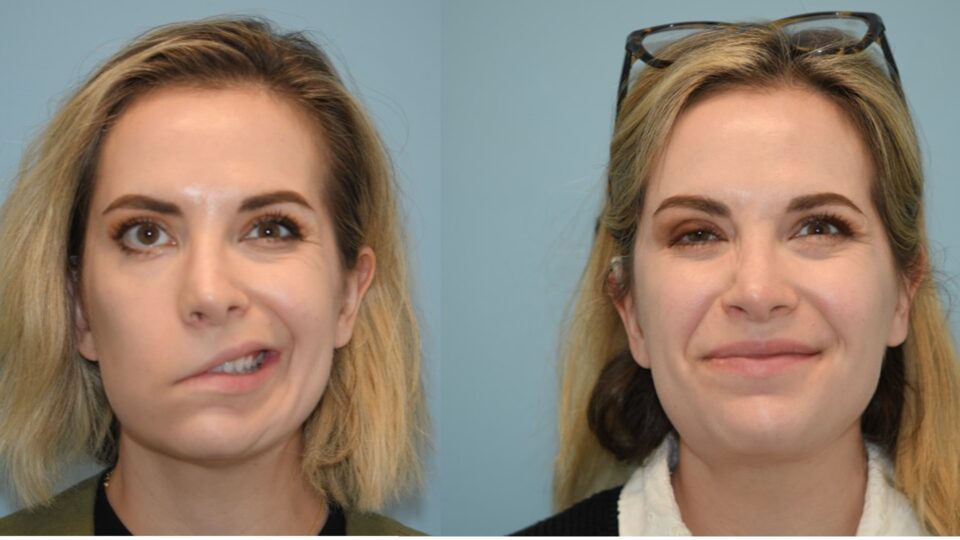
Patients with single-sided deafness (SSD) now make up our fastest-growing cohort. These patients often experience sudden idiopathic sensorineural hearing loss, and we don’t know exactly what causes it. I would say 30 percent of the patients that we implant are adults with SSD, and our cochlear implants in this group have been wildly successful.
Dr. McMenomey: We also started implanting pediatric patients who have SSD. They may be born with an anatomical variant: maybe their cochlea isn’t developed enough or their cochlear nerve is not robust enough to carry a signal. We’re seeing some success here as well, though not to same level as in adults who could hear before experiencing SSD.
Removing Age as a Limitation
Physician Focus: What accounts for the center’s huge range in patient ages?
Dr. Shapiro: Dr. Roland devised a protocol that allows us to offer cochlear implants under local anesthesia with sedation to patients who are older or have extensive comorbidities. The patient is awake but sedated, and the recovery is much quicker than from general anesthesia. Anyone who is medically fragile or older, like the 97-year-old patient, could have the surgery with local anesthesia—that’s a big deal because not a lot of centers do that.
“There really is no age limit.”
William H. Shapiro, AUD
We also implant patients routinely at 6 months of age, putting in two implants at the same time. Official FDA approval is down to 9 months of age, but a physician who thinks it’s in the best interest of the patient can implant off-label at earlier ages. The 4-month-old child that we implanted had bacterial meningitis, which can cause the tunnels in the cochlea to ossify. It’s important to get the electrode in as quickly as possible or it won’t be possible to place the full array. So that child needed implants at 4 months of age—there really is no age limit.
Expertise with Auditory Brainstem Implants
Physician Focus: The center has played a leading role in advancing auditory brainstem implants (ABIs). Can you tell us about the center’s expertise with ABIs and explain what constitutes a successful case?
Dr. Shapiro: There are two cohorts that we commonly treat with ABIs. The first cohort is adult patients with neurofibromatosis type 2 from whom Sean needs to remove a tumor. Potential hearing loss is always a consideration with operations to remove these kinds of tumors. The other cohort is children who are born with no cochlea or cochlear nerves—Dr. Susan B. Waltzman has played a leading role in advancing ABIs in this group.
In our experience, most children receive a measurable degree of auditory benefit from their implant, as well as improved quality of life. Our best pediatric performers have some limited open-set discrimination, which means they’re able to understand some speech without additional visual cues. None of our patients who receive ABIs use audition as their primary mode of communication; they’re all what we call multimodality: they also use sign language, lipreading, or other strategies.
Dr. McMenomey: It depends on the year, but we perform between 5 and 10 ABIs every year. When we put an ABI in, it’s because there’s no other option. The children who were born without a cochlea or without a nerve aren’t candidates for cochlear implants, so their options are either an ABI or remaining without hearing.
Preserving Hearing in Skull Base Surgery
Physician Focus: The center has worked hard to minimize hearing loss following skull base surgery—a big concern for patients. What lessons have you learned from that experience?
Dr. McMenomey: The most common skull base surgery is for acoustic neuroma, also known as vestibular schwannoma, a typically benign tumor on the vestibular nerve. This tumor usually causes unilateral hearing loss due to its location inside the skull, where it can exert pressure on the auditory nerve. Hearing loss is far and away the most common symptom. Fortunately, we do have options to help this group of patients deal with their hearing loss.
Our goal is—whenever possible—to preserve hearing, to keep it right where it is preoperatively by preventing further damage to the brain and nerve. We have conducted several studies to understand how factors such as acoustic tumor size impact hearing loss, enabling us to better advise and manage patients undergoing these surgeries.
Dr. Shapiro: If you have a patient who comes in with normal hearing but who has an acoustic neuroma, they may lose their hearing in one ear when the neuroma is removed. But if the surgeon feels that they saved the nerve, we may be able to implant that patient with a cochlear implant. In fact, we’ve done that for some of our neuroma patients with SSD, including patients with stable unoperated tumors.
Innovations on the Horizon
Physician Focus: What ongoing research at the center do you find particularly exciting?
Dr. McMenomey: For the last hundred years, there really hasn’t been a nonsurgical way to repair a perforated eardrum. But we are doing a study right now that is looking at applying growth factor to the eardrum. It’s a double-blind study, and some patients are getting a placebo and some patients are getting the active drug to answer this question: Is there a way we can repair a perforated eardrum without taking patients to the operating room?
“The coming decades promise exciting advancements in cochlear technology, and we’re thrilled to contribute to these efforts.”
Sean O. McMenomey, MD
Another study we’re involved in is exploring whether we can create an electrode that continuously bathes the cochlea in steroids, preventing an inflammatory reaction to the presence of a foreign body—the implant—within the cochlea and thereby preserving hearing. The answer is not in yet, but it’s ongoing work.
Finally, the center is conducting experimental cochlear implant mapping based on music perception in patients with SSD. Again, the research shows how we’re leading the way in investigating different strategies, in this case helping patients with implants appreciate music.
One of the things that makes it so fun to work here is that NYU Langone is basically involved in every cutting-edge cochlear implant trial, because we’re a high-volume center and well known and we do good work. The coming decades promise exciting advancements in cochlear technology, and we’re thrilled to contribute to these efforts.