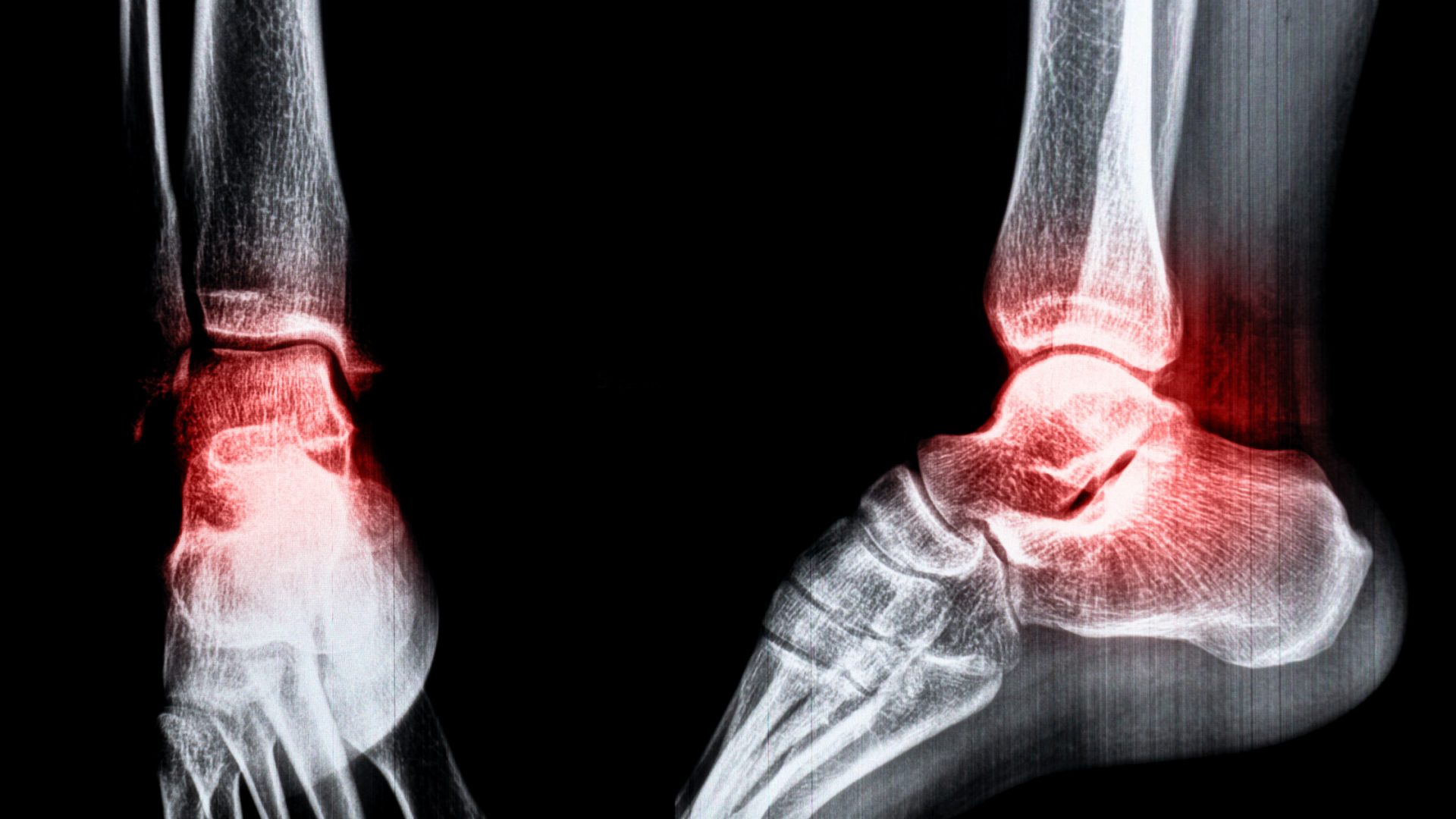
Osteochondral lesions of the talus often result in early-onset osteoarthritis in the ankle joint if left untreated. Due to the avascular nature of articular cartilage, which limits its healing capacity, these ankle injuries are typically managed through surgical intervention.
However, surgical treatments alone often lead to the formation of fibrocartilage, which is less tribologically and mechanically robust compared to the native hyaline cartilage of the joint. Consequently, biologic adjuvants are increasingly being explored for their potential to enhance cartilage healing and promote a hyaline-like quality. In 2017, at the inaugural International Consensus Meeting on Cartilage Repair of the Ankle, it was agreed that certain biologic adjuvants could be considered as part of a conservative management strategy for treating these ankle lesions.
“Medicine is constantly evolving and improving. We still have to do quality basic science and clinical studies to show that these biologics are effective,” says NYU Langone orthopedic surgeon John G. Kennedy, MD. “Once efficacy is confirmed, biologics will help in sports injuries and in arthroscopy. We’re still going to operate. It’s just that now we’ll have new tools to promote regeneration and repair.”
“Once efficacy is confirmed, biologics will help in sports injuries and in arthroscopy. We’ll have new tools to promote regeneration and repair.”
John G. Kennedy, MD
To help surgeons sort through the expanding roster of adjuvants for ankle cartilage injuries, Dr. Kennedy and a collaborator highlighted some of the most promising options in the Journal of the American Academy of Orthopaedic Surgeons.
Platelet-Rich Plasma
NYU Langone’s Foot and Ankle Center has long used platelet-rich plasma (PRP), an autologous product that is not only a potent anti-inflammatory but also a downregulator of metalloproteinases. Through that activity, PRP can help control joint homeostasis and stop cartilage destruction.
Dr. Kennedy’s team has shown that a single in-office PRP injection is as effective as serial injections for giving patients with small chondral defects some symptomatic relief.
He cautions, however, that the adjuvant doesn’t contain stem cells, contrary to some claims, and is more chondroprotective than chondrogenic. “It doesn’t produce a new joint or new cartilage,” he says, “but in small areas you can certainly affect your fibrocartilage infill, which may be helpful in the short term or medium term.”
Concentrated Bone Marrow Aspirate
Concentrated bone marrow aspirate (CBMA), another widely used biologic, is typically extracted from a patient’s pelvic bone in an operating room, centrifuged, and then injected into the ankle joint. Unlike PRP, Dr. Kennedy says, CBMA contains a small quantity of stem cells.
In the context of the joint, researchers believe that injected stem cells can be engulfed by macrophages or monocytes, which then become activated and contribute to a biological milieu known as the secretome. In the right environment, the secretome can have chondrogenic, chondroprotective, immune modulatory, and antibacterial effects.
“We’ve been pushing the envelope to better characterize what’s truly in the secretome and whether we can predict the clinical effect.”
“There are multiple downstream effects of a secretome within a joint, which is a much greater effect than we previously thought about these stem cells,” Dr. Kennedy says. “That’s a very exciting area of work here at NYU Langone: we’ve been pushing the envelope to better characterize what’s truly in the secretome and whether we can predict the clinical effect from patient to patient based on the spectrum of what they have in their bone marrow.”
Micronized Adipose Tissue
Based on research suggesting that fat cells can be chondrogenic, NYU Langone’s orthopedic surgeons have also been assessing micronized adipose tissue as a potential solution for post-traumatic osteoarthritis in the ankle joint.
In the first study of its kind in the United States, Dr. Kennedy and colleagues showed that injected fat cells are safe and potentially beneficial in patients with post-traumatic osteoarthritis of the ankle. The micronized adipose tissue, he suspects, contains additional factors that may add to the effect.
The team is investigating different formulations to increase the strategy’s effectiveness, and has seen promising results in patients with knee osteoarthritis as well. “We’re not growing new joints. We’re simply protecting that joint, removing the cause of the symptoms, and prolonging the life of the joint for as long as we can,” Dr. Kennedy says.
Hyaluronic Acid and Other Injectables
Another biologic, hyaluronic acid, acts like a chondroprotective adjunct with some added anti-inflammatory and chondrogenic properties when injected into the knee joint. “We use it as an adjunct to many cases involving an osteochondral lesion or long-term post-traumatic osteoarthritis, and the results of that are very encouraging,” Dr. Kennedy says.
In addition, the medical center’s orthopedic researchers are collaborating on investigations of other injectable agents, like a lubricin mimetic. “Lubricin is the true WD-40 of the joint,” Dr. Kennedy says.
“The whole aspect of regeneration coupled with the preservation of existing cartilage is massively exciting for the future.”
Ongoing clinical trials are assessing the effectiveness of a recombinant protein that mimics lubricin’s properties. “I think that’s going to be the next great breakthrough in terms of prolonging the life of many of these arthritic joints,” he says.
As an acknowledged leader in the field, NYU Langone will host the 2025 International Consensus Meeting on Cartilage Repair of the Ankle to review the latest progress and clinical results from around the world.
“I think we’re really at the tip of the spear in many of these chondrogenic and chondroprotective biologics,” Dr. Kennedy says. “The whole aspect of regeneration coupled with the preservation of existing cartilage, to me, is massively exciting for the future.”