Referral Notes:
- Marking a first in the nation, NYU Langone surgeons have pioneered a minimally invasive technique to address urethral damage caused by radiation.
- The surgical method leverages two innovative robotic systems, incorporating free flaps from the small bowel and new blood vessels.
- Four patients have been treated to date, all with promising early outcomes; submissions to major conferences in urology and plastic surgery are planned for this year.
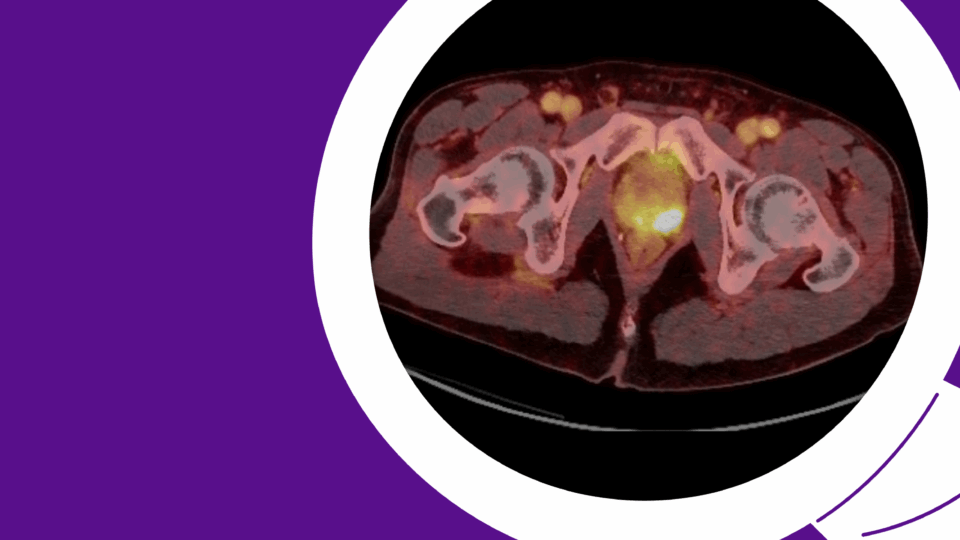
While radiation therapy (RT) stands out as a highly effective treatment for localized prostate cancer, a significant drawback is the risk of injury to healthy cells in the surrounding tissue. Existing on a spectrum, urethral damage caused by radiation is among the most detrimental urological complications.
Nearly two decades ago, while in his residency, urologic surgeon Lee C. Zhao, MD, director of male reconstructive surgery for the NYU Langone Health system, encountered this complication for the first time. Since then, he has dedicated his career to developing a solution.
“Because of impaired tissue healing after RT, urine can leak into the pelvic bone, causing recurrent infections, pelvic pain, and impaired ambulation,” says Dr. Zhao.
Dr. Zhao and colleagues, including Jamie P. Levine, MD, chief of microsurgery, have developed the nation’s first minimally invasive technique to address urethral damage caused by radiation. So far, the procedure has been successfully completed in four patients, all of whom had debilitating symptoms.
“I’ve spent my entire career trying to solve this problem,” Dr. Zhao says. “At long last, we have come up with a solution.”
Pioneering the Technique
The approach combines two innovative surgical systems, the Da Vinci single-port robot and the Symani Surgical System, with the expertise and collaboration of both urologic and plastic surgery.
Dr. Zhao explains that the primary operative hurdle when treating these injuries is joining the bladder and urethra after removing damaged tissue; in most cases, the distance is too great to rejoin the tissue directly, and standard reconstructive techniques have proven unsuccessful. The only other option is to remove the bladder entirely, which is unappealing to most young, physically fit patients.
“I’ve spent my entire career trying to solve this problem. At long last, we have come up with a solution.”
Lee C. Zhao, MD
According to Dr. Zhao, the breakthrough lies in the application of free tissue transfer, specifically the transfer of a segment of tissue from the small bowel deep into the pelvis, then using robotic microsurgery to connect new blood vessels.
“It is difficult to bring tissue deep into the pelvis, while also connecting the new blood vessels,” says Dr. Zhao. “This new robotic technique allows us to bring the blood vessels further into the pelvis, ensuring a transferred flap of tissue can survive.”
Dr. Zhao notes that small bowel tissue is advantageous because it enables the passage of urine more easily than other types of tissue, making it particularly effective for urological procedures.
He and his team have been progressing toward the ileal free flap for radiation injury by first applying the approach in the context of urethral trauma. “The main difference is that now we are doing this deep in the pelvis, for which we need the robotic technology,” Dr. Zhao says.
Currently, the ideal surgical candidate is someone with a history of locoregional prostate cancer or other pelvic malignancy who has received RT by itself or surgery and RT. In some patients, the combination of surgery and RT leaves scar tissue in the urethra, causing urine to leak outside of the urinary tract into the pelvic bone.
Nationwide Referrals, Disseminating Results
The first patient underwent the procedure in August 2024, and it was carried out successfully.
Prior to the surgery, the patient struggled to ambulate and relied heavily on a walker for assistance. He had previously undergone multiple procedures to restore continence, all of which failed. “Our first patient suffered with complications for over a decade,” says Dr. Zhao. “He had considerable pain caused by the ongoing urine leakage.”
“We hope to present a small case series shortly. The early results have been phenomenal.”
Remarkably, just two weeks after surgery, the patient could walk independently and even went on a camping trip. “The speed of recovery was astonishing,” says Dr. Zhao. “Enabling a person to reclaim their life and participate in their favorite activity was truly rewarding.”
Given the early success, Drs. Zhao and Levine report that patients are traveling from across the country to undergo the procedure. They plan to share their initial experiences at conferences in urology and plastic surgery this year.
“We hope to present a small case series shortly,” says Dr. Zhao. “The early results have been phenomenal. We believe it is effective in relieving pain and restoring the function of the urinary tract.”
He adds, “It is a great option for otherwise healthy patients who want to maintain their quality of life; the only other option is removal of the bladder.”