Referral Notes:
- HNS is shown to be comparable to CPAP as a safe and effective treatment for obstructive sleep apnea, yet usage remains limited.
- NYU Langone clinicians have developed a novel institutional approach to ensure that patients eligible for HNS are able to receive the treatment and achieve positive outcomes.
- Physicians throughout the health system and referring providers are encouraged to contact the sleep otolaryngology team for potential candidates.
- Specially trained surgeons evaluate patients, perform the implantation procedure, and customize device settings to optimize results.
The gold standard therapy for obstructive sleep apnea, continuous positive airway pressure (CPAP), is highly effective, yet it can be so uncomfortable that roughly 50 percent of patients are nonadherent. Recently, however, an alternative has emerged: hypoglossal nerve stimulation (HNS), delivered through a surgical implant. Its efficacy is comparable to CPAP, and its tolerability is superior.
The sole HNS implant available in the United States is the Inspire device, approved by the FDA in 2014. Although it brings robust results in terms of treatment outcomes and patient adherence, usage remains limited; about 75,000 people have received an Inspire implant worldwide, compared with the millions who use CPAP.
One major barrier to adoption arises from the technical complexities associated with the implantation.
“This is a very detailed surgery, and there’s a limited pool of surgeons with the skill set to do it,” says Erich P. Voigt, MD, director of the Division of General Otolaryngology and Sleep Surgery at NYU Langone Health. “That expertise extends to proper patient selection and extensive post-surgical follow-up, both of which are key to successful outcomes.”
“There’s a limited pool of surgeons with the skill set to do the surgery. That expertise extends to proper patient selection and extensive postsurgical follow-up.”
Erich P. Voigt, MD
To address these challenges, Dr. Voigt and colleagues have developed a coordinated, multidisciplinary approach aimed at ensuring that patients get the opportunity to benefit from the device—and that they achieve optimal results.
Enhancing Patient Selection
The Inspire is recommended for two broad categories of apnea sufferers: adults with a body mass index of at most 40 who cannot tolerate CPAP and who aren’t candidates for other standard-of-care treatments, as well as pediatric patients with Down syndrome.
Identifying eligible patients is not always straightforward. The device is contraindicated, for example, in those whose breathing during sleep is impaired primarily by skeletal anomalies or collapse of the soft palate. “The patient’s anatomy is crucial to choosing the correct treatment,” Dr. Voigt notes.
At NYU Langone, physicians throughout the health system are encouraged to message the sleep otolaryngology team via Epic if they think a patient is a likely candidate for HNS. A team member then performs a sleep endoscopy to determine the site of the obstruction. If the test shows the tongue blocking the airway, patients are offered the Inspire as a treatment option. If not, they are referred for an appropriate procedure, such as mandibular advancement surgery or uvulopalatopharyngoplasty.
Providers outside NYU Langone are also welcome to contact the team to discuss patient referrals.
Refer a Patient Today: If you have a patient who could benefit from our specialized sleep apnea care, we’re here to help. Call 646-501-7890 (Manhattan office) or 516-682-8288 (Long Island office) to refer a patient to the sleep otolaryngology team or learn more about our services.
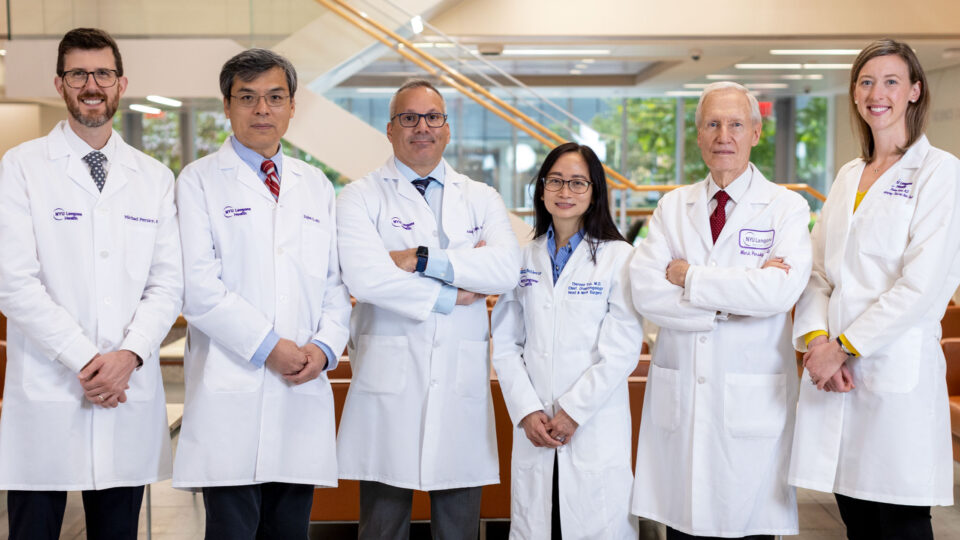
This kind of integrated approach is rare outside of the most advanced academic sleep medicine centers. Dr. Voigt, who has led the otolaryngology division since 2016, was a pioneer in administering the Inspire in the context of a multidisciplinary sleep otolaryngology practice.
“Prior to coming here, I saw patients whose obstructive sleep apnea had been evaluated by specialists working in silos—neurologists, pulmonologists, maxillofacial surgeons, dentists—and who’d received therapies that were frequently not effective,” he says. “I wanted to create a center where all the specialties come together and find the right therapy for the right patient.”
“I wanted to create a center where all the specialties come together and find the right therapy for the right patient.”
In addition to Dr. Voigt, two other specially trained surgeons perform the Inspire implantation at NYU Langone—Courtney Chou, MD, and Nikhita Jain, MD. Both were recently recruited, in part, to meet rising demand for the procedure.
Prioritizing Patient–Physician Communication
One important element in NYU Langone’s approach to HNS is fostering the patient’s participation in the decision-making process. “Not everyone wants a device implanted into their body,” Dr. Voigt observes. Such reservations often vanish, however, after a discussion of the Inspire’s risks and potential benefits.
Although those risks include scarring of the incision areas and muscle weakness that can impair speech and swallowing, major adverse effects are rare. By contrast, uncontrolled sleep apnea heightens patients’ risk of health problems, including cardiovascular disease, pulmonary hypertension, atrial fibrillation, obesity, cognitive deficits, chronic fatigue, and vehicular accidents.
Dr. Voigt and his team review these considerations with each candidate for the Inspire, along with the details of the surgery and the postoperative experience.
“An informed patient is the best patient,” he says. “They’re prepared for all aspects of the procedure, and they know what to look out for so that we can catch any complications quickly.”
Customizing Treatment to Maximize Benefits
The device comprises three components: a sensing lead, situated near the ribs; a pulse generator, placed below the collarbone; and a cuff electrode, which fits around a branch of the hypoglossal nerve. Whenever the sleeping patient takes a breath, the sensor signals the generator to send an impulse to the electrode, which triggers the tongue to clear the airway. A handheld remote is used to turn the device on and off, adjust stimulation intensity, and set the timing of stimulation onset.
“Three months after the surgery, [the patient] told us, ‘I’m going back into the workforce.’ That’s an example of what this treatment can do.”
The 90-minute surgery involves microneural dissection with real-time stimulation to find the nerve branches that push the patient’s tongue forward. “Once we’ve identified those branches, we place an electrode with three contact points, enabling the device to control tongue movement precisely,” Dr. Voigt explains.
Most patients are discharged home the same day. A month later, they return to have the device activated. Stimulation is initially set at minimal intensity, with the dose titrated upward by one level each week. When the stimulation becomes strong enough to awaken the user, the setting is turned down a notch. At that level, patients typically report feeling more rested during the day than at baseline, and diagnostic sleep studies show significant improvements in apnea symptoms.
Among the team’s success stories is a woman who was implanted at age 65. “When she came to us, she was so exhausted that she planned to retire from her job,” Dr. Voigt recalls. “Three months after the surgery, she told us, ‘I’m going back into the workforce. I have my energy back. I have my desire to live back.’ That’s an example of what this treatment can do.”