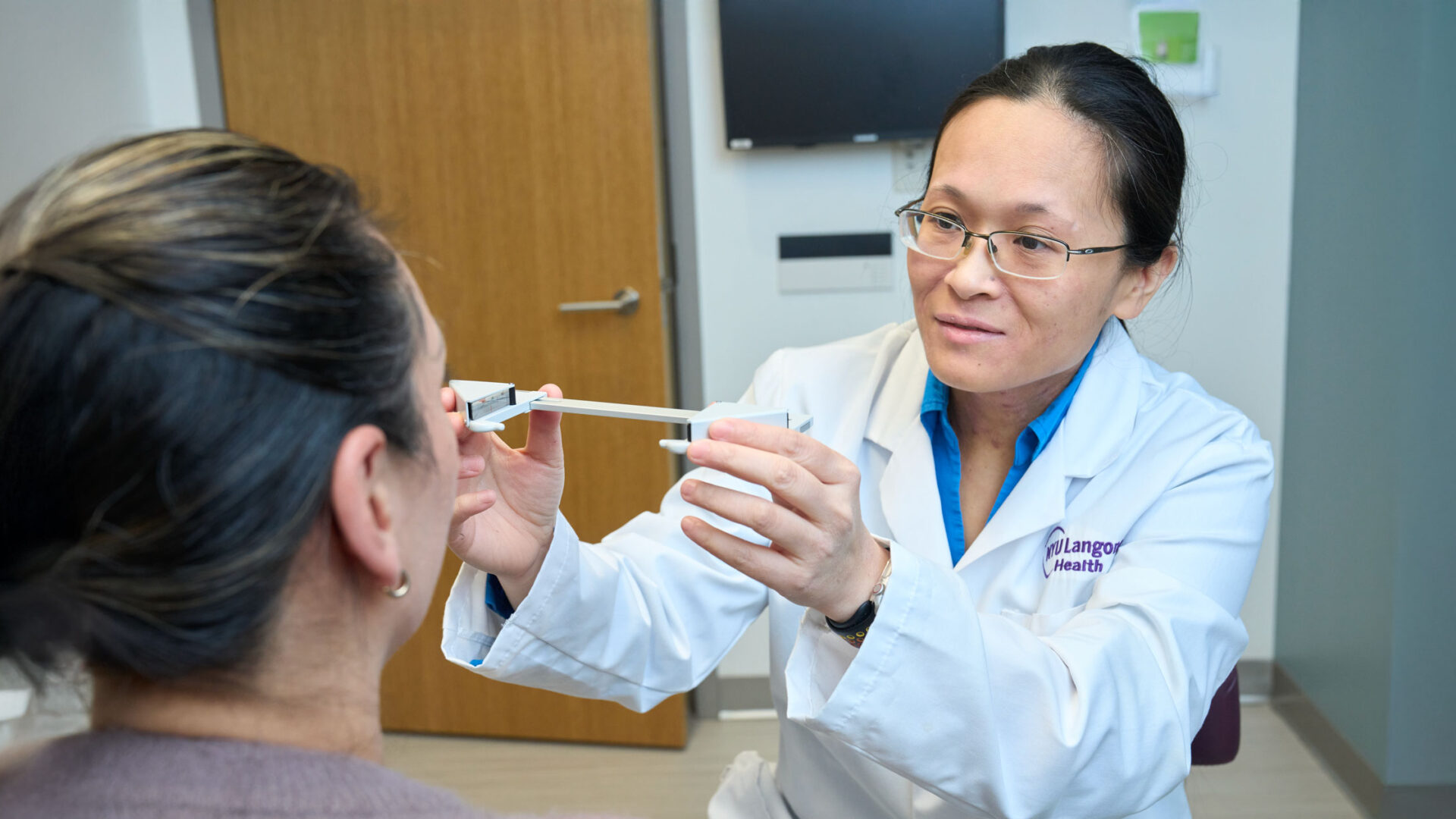
Oculoplastic and orbital eye surgeon Roxana Fu, MD, has joined NYU Langone Health’s Department of Ophthalmology as chief of oculoplastics. She is also a clinical associate professor of ophthalmology in the department.
Dr. Fu has been at the forefront of driving innovation in the treatment of disorders of the eyelid, the tear duct drainage system, and orbit in adults and children, leading studies that apply artificial intelligence (AI) and machine learning techniques to optimize ophthalmologic surgical practice.
Here, Dr. Fu shares her goals as chief and her current and upcoming research initiatives.
Physician Focus: What drew you to take on this role at NYU Langone, and what are your top priorities as chief of oculoplastics?
Dr. Fu: When you set foot in New York, you feel like anything is possible. On top of that, the environment at NYU Langone boosts your professional growth exponentially. The culture of high productivity fostered by our chair, Kathryn A. Colby, MD, PhD, is truly inspiring. We roll up our sleeves and get things done—no task is beneath us.
“The culture of high productivity fostered by our chair is truly inspiring. We roll up our sleeves and get things done.”
Roxana Fu, MD
My primary focus will be delivering exceptional patient care. By fostering meaningful collaborations across the variety of subspecialties that intersect with oculoplastic surgery, this goal will be achieved.
Beyond patient care, I’m part of a group of oculoplastic surgeons investigating the automation of radiographic surgical indicators for pediatric orbital abscess. We hold a $2.8 million grant from the National Eye Institute (NEI) to support this work. Together, we’re utilizing AI and machine learning techniques to improve patient selection for various surgical approaches using a comprehensive imaging database. This project will continue at NYU Langone.
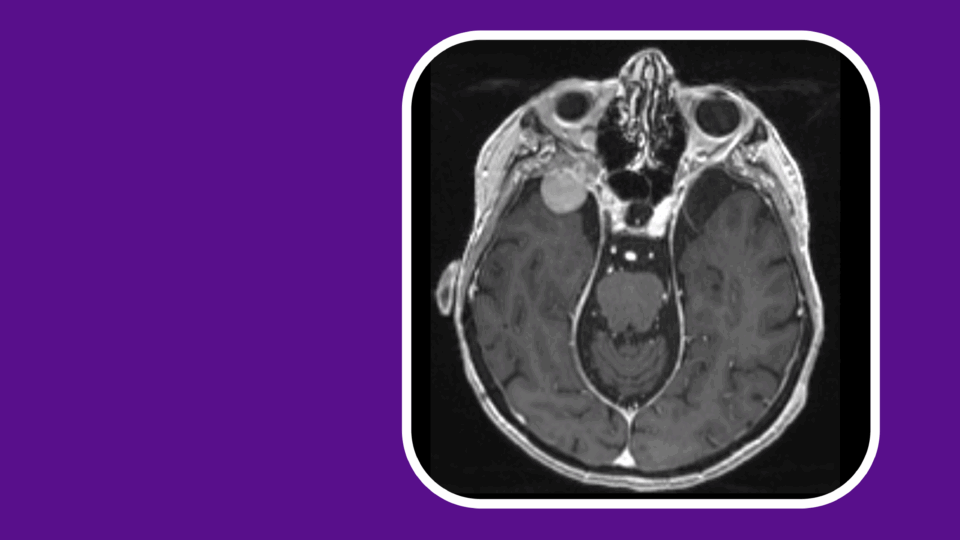
Physician Focus: As part of that research, you published a retrospective study suggesting that AI-generated proptosis measurements may help identify patients who require orbital abscess surgery. Why are these results important, and what’s next for this work?
Dr. Fu: Orbital cellulitis is a relatively common complication of sinus infection, especially in children. Surprisingly to some, it can lead to a host of serious complications, including the formation of an orbital abscess and blindness. Proptosis—or bulging eyes—is a consistent marker of orbital cellulitis, but can be challenging to measure clinically, so we investigated the use of computed tomography (CT) scanning to improve these measurements.
In the current literature, surgical indications for orbital abscess drainage in pediatric populations are poorly defined. Pressure from an abscess can damage the optic nerve and increase the risk of blindness, making it crucial to identify patients needing immediate surgery. The goal of our study was to use AI to automate various CT measurements and evaluate any association with the need for eventual surgery.
“We found that the AI software measures of proptosis showed a good overall ability to predict the need for eventual surgery.”
We found that the AI software measures of proptosis significantly differed from physician evaluations and showed a good overall ability to predict the need for eventual surgery. In addition, the software measures were significantly higher in the early-surgical subgroups compared to the late-surgical subgroups, with physician measurements unable to meaningfully differentiate between these subgroups.
Based on these findings, we plan to conduct larger studies to better define radiographic markers to assess pediatric patients with orbital abscess.
Physician Focus: Why did you choose to focus on children with orbital abscess?
Dr. Fu: When I was in training, I witnessed a 12-year-old boy go blind in one eye while being transferred to our hospital in an ambulance. After developing a cold, he developed a sinus infection that eventually spread to his eye, causing a rapid rise in eye pressure. That young man was in Junior ROTC. He had aspirations to pursue a career that required binocularity. Sadly, because he got a cold, suddenly that option is off the table.
This patient left a lasting impression on me—sudden vision loss like this should not happen in children. Using AI, we want to identify kids with orbital cellulitis that are at high risk for complications, and hopefully be able to better triage their care.